Suture Needle Basics
By: Nechama Brilliant, BSN, RN, CNOR
Published: 3/13/2024
Suture needles come in various sizes, shapes, and diameters. The surgeon will choose suture needles based on the procedure type, location of the surgical incision, and tissue type. Each type of needle has a special purpose and is useful for different applications. Heavier needles are used for thicker tissue and muscle, whereas finer needles are used for delicate tissue.
Needle Anatomy
Needles have three main parts: the swage, the body, and the tip (Figure 1). The swage is the area where the suture and needle meet. With some swaged needles, the suture needs to be cut away from the needle, while with other swaged needles, the suture strand can be popped off the needle without the use of scissors. The body of the needle can be round in diameter, have angled edges, or be flat. The body of the needle ends in a point. The point can be tapered, blunt, or triangular.1
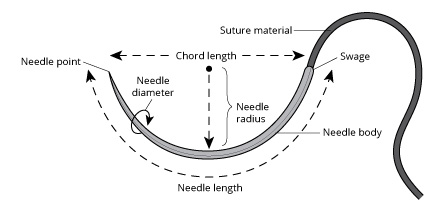
Figure 1. Suture needle.
Handling Needles
Suture needles should remain in the original packaging until the time of use. When the suture is needed, the appropriate size needle holder should be chosen to grasp the suture needle and remove it from the package (Figure 2). The needle holder should grasp the suture needle approximately one-third of the distance from the swaged edge (Figure 3). Care should be taken when handing the loaded needle holder to the surgeon.

Figure 2. Suture needle removed from package.
Figure 3. Needle holder.
Needle Safety
AORN recommends that the sterile field be maintained in a way that allows for observable awareness of all sharps, including suture needles. The integrity of the suture needle should be monitored from the time the needle is added to the sterile field and throughout the entire procedure. Suture needles should be counted audibly and visibly viewed by the scrub person and nurse. The needle count should be performed and displayed in a standardized fashion in accordance with organizational policy. After the procedure, all sharps should be disposed of in adherence with the Occupational Safety and Health Administration Bloodborne Pathogens Standard.2,3
References
- Cromb MM. Sutures, sharps, and instruments. In: Rothrock JC, ed. Alexander’s Care of the Patient in Surgery. 17th ed. St Louis, MO: Elsevier; 2023:174-198.
- Guidelines for sharps safety. In: Guidelines for Perioperative Practice. Denver, CO: AORN, Inc; 2024.
- 29 CFR 1910.1030 Bloodborne Pathogens Standards. Occupational Safety and Health Administration. 1910.1030 - Bloodborne pathogens. | Occupational Safety and Health Administration (osha.gov)
AORN Resources
AORN members can access:
- Preventing Perioperative Sharps Injuries - AORN Journal
- Understanding Causes of Needlestick and Other Sharps Injuries Among OR Personnel - AORN Journal
- Guidelines in Practice: Sharps Safety - AORN Journal
- Sharps Safety Guideline Essentials | AORN
- Sharps Safety FAQs | AORN

