Small Bowel Resection
By: Adapted from eGuidelines+ by Valerie Komoroski, MSN, RN, CNOR, CNIV
Published: 10/25/2023
Indications for Procedure
A small bowel resection involves removing diseased portions of the small intestine through an abdominal incision and reconnecting the remaining tissue. It is indicated to remove disease or damaged tissue caused by an intestinal tumor; an obstruction; or ulcerated, damaged, or necrotic tissue caused by Crohn disease, adhesions, or a volvulus.1
Patient Positioning
Patient positioning is based on surgeon preference, but usually patients are placed in the supine position with their arms extended and palms up on arm boards and angled less than 90 degrees or with their arms tucked inward.1 Care must be taken to prevent injury and interference with monitoring equipment.2 Because each surgeon has their own preferences for equipment placement and positioning, it is important to ensure that the patient’s arms, hands, and feet are protected and not going to be pressed against or crushed with equipment.
Surgical Prep
- Although each surgeon’s preference for antisepsis varies, the manufacturer’s instructions for use should be followed.
- Begin the prep at the umbilicus using sterile cotton-tipped swabs dipped in antiseptic solution. Discard the swabs after use.
- Have extra swabs available should the need arise.
- Following the manufacturer’s instructions for use, the prep should cover the nipple line to the pubis, and bedside to bedside, beginning at the incision site and moving outward, with generous borders in case the surgeon needs to extend the incision.1,3

Equipment Needed
- Electrocautery unit
- Suction unit
- Fluid warmer
- Sequential compression device unit, if indicated and ordered
- Laparotomy instrument set to include handheld retractors (eg, Harrington, Richardson, Army Navy, malleable), forceps (eg, DeBakey, Russian, Singley), scissors (eg, Mayo, Metzenbaum), and various needle holders and clamps (eg, Allis, Babcock, Crile, intestinal).
- Self-retaining retractor or table-mounted retractor of the surgeon’s preference (eg, Balfour, Thompson)
Be sure to have longer instruments available for deeper body cavities.
Supplies Needed
- Lap sponges
- Electrocautery pencil
- Extended electrocautery tip
- Scalpel blade #10 or #15
- Grounding pad
- Dissectors
- Vessel loops
- Various staplers and reloads
- Clamp covers
- Suture booties
- Adhesive barrier and ostomy supplies
Suture
The surgeon’s preference of absorbable suture is used for the peritoneum and muscle. Nonabsorbable sutures are used for the fascia. Absorbable sutures or staples are used for skin.
Dressing
The surgeon’s preference for dressing is used and may include gauze with tape or border dressing. A colostomy bag may be needed.
Basic Procedure Workflow
To perform a small bowel resection, the surgeon will
- Incise the skin, fascia, muscles, and peritoneum through a midline incision using a #10 blade.
- Control hemostasis with ligatures or electrocoagulation.
- Obtain retraction throughout each layer using an appropriate surgical tool.
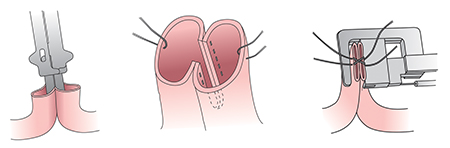
- After the small bowel is reached, place clamps above and below the diseased portion to be removed.
- Reconnect the small intestine via an end-to-end, end-to-side, or side-to-side anastomosis using a stapling device or suture (surgeon’s choice).1
- Close skin with the staples or suture (surgeon’s choice).
Related Procedures
Procedures that may be performed in combination with a small bowel resection include
- Ileostomy and jejunostomy, in which a temporary or permanent opening is created to divert feces to the outside of the body, alleviating large bowel activity.
- Intestinal transplantation, in which donor tissue is connected to the recipient’s stomach, duodenum, or jejunum and remaining colon to extend the length of the intestine. This will increase the absorptive capacity for patients with short-gut syndrome, especially those who can no longer receive parenteral nutrition.1
Procedural Variations
The surgeon may opt to perform small bowel resection laparoscopically if the patient is eligible. Certain types of cancer, obesity, prior abdominal surgery, anatomy variations, or other diseases may preclude the patient from being a good candidate for a laparoscopic approach.
Postoperative Recovery
Postoperative ileus, also called paralytic ileus, involves impaired intestinal motility and typically occurs for three to six days after the procedure, but it may persist beyond six days. It may be caused by handling/disturbing the tissue itself or opioids used to treat procedural pain. Symptoms may include bloating, pain, nausea, emesis, or a feeling of fullness. A postoperative ileus may result in exacerbated nausea and vomiting, bowel obstruction, or prolonged hospitalization.4
Patients undergoing intraperitoneal procedures have an increased risk for developing an adhesive small bowel obstruction. In this condition, fibrous bands develop between abdominal tissues or organs that can cause abdominal pain and intestinal obstruction and may require additional surgery. Minimal handling of tissue during surgery and the use of antiadhesive barriers can help prevent formation of adhesions.5
Editor's note: This content is adapted from AORN eGuidelines+. If your facility subscribes to eGuidelines+, you can access the full content.
References
- Neil JA. Gastrointestinal surgery. In: Rothrock JC, McEwen DR, eds. Alexander’s Care of the Patient in Surgery. 15th ed. St. Louis, MO: Elsevier Mosby; 2015:334-335.
- Denholm B. Clinical Issues. AORN J. 2009;89(4):755-757.
- Best practice guidelines: surgical skin preparation. Winnipeg Regional Health Authority. http://www.wrha.mb.ca/extranet/eipt/files/EIPT-005-001.pdf. Accessed January 28, 2023.
- Carter S. The surgical team and outcomes management; focus on postoperative ileus. J Perianesth Nurs. 2006;21(2A Suppl):S2-S6.
- Catena F, DiSaverio S, Coccolini F et al., Adhesive small bowel adhesions obstruction: evolutions in diagnosis, management and prevention. World J Gastrointest Surg. 2016;8(3):222-231.
AORN Resources
AORN members can access:
- Patient Skin Antisepsis and Patient Positioning | AORN Guideline Essentials
- Patient Skin Antisepsis and Patient Positioning | AORN FAQs
If your facility subscribes to eGuidelines+, you can access:
- Instruments at a Glance | AORN eGuidelines+
- Positioning at a Glance | AORN eGuidelines+
- Procedures at a Glance | AORN eGuidelines+
- Room Setup at a Glance | AORN eGuidelines+
- Skin Prep at a Glance | AORN eGuidelines+
- Patient Skin Antisepsis Guideline | AORN eGuidelines+
- Positioning the Patient Guideline | AORN eGuidelines+

