Laparoscopic Cholecystectomy
By: Adapted from eGuidelines+ by Valerie Komoroski, MSN, RN, CNOR, CNIV
Published: 8/30/2023
Indications for Procedure
Laparoscopic cholecystectomy is indicated for acute cholecystitis; symptomatic cholelithiasis, including complications related to common bile duct and cystic duct stones with the possibility of pancreatitis; and biliary dyskinesia (abnormal gallbladder emptying without obstruction).1
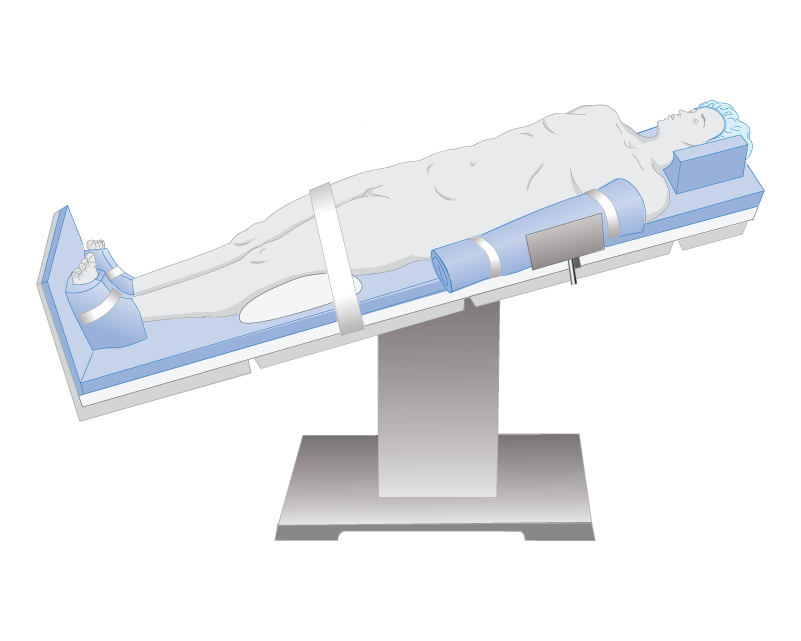
Patient Positioning
Patients are usually placed in the supine position, with variations of reverse Trendelenburg and lateral tilt with the right side up. Some surgeons may want a split leg table to stand between the legs.1,2 The patient should be on an OR bed that a C-arm could fit under in the event an intraoperative cholangiogram would be needed to check for stones.
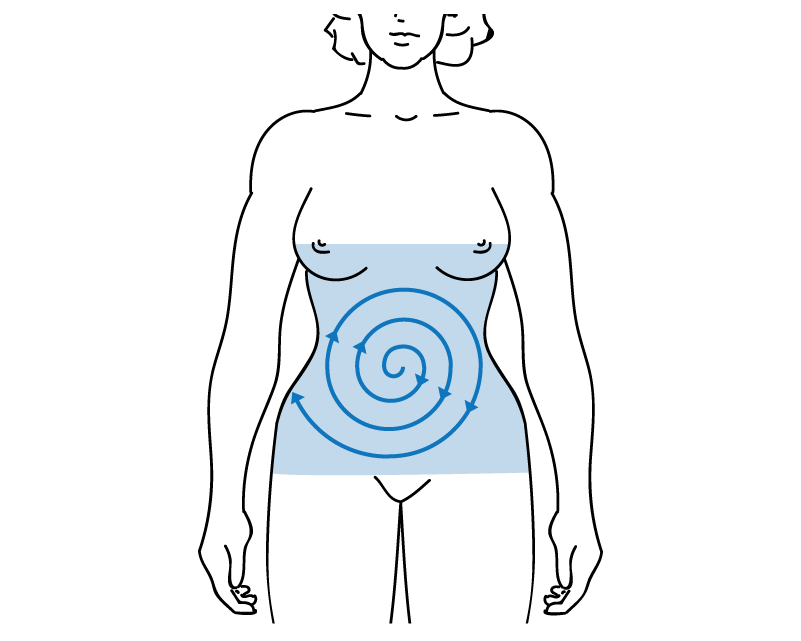
Surgical Prep
Although each surgeon’s preference for antisepsis varies, the manufacturer’s instructions for use should be followed.
- Begin the prep at the umbilicus using sterile cotton-tipped swabs dipped in antiseptic solution. Discard the swabs after use.
- Have extra swabs available should the need arise.
Following the manufacturer’s instructions for use, the prep should cover the nipple line to the pubis, and bedside to bedside, beginning at the incision site and moving outward.
Equipment Needed
- Video tower/monitors
- Camera and lenses
- CO2 gas and insufflator (maximum pressure of 15 mm Hg)
- Electrocautery unit
- Suction
- Sequential compression device unit, if indicated/ordered
- Laparoscopic and general surgical instruments


Supplies Needed
- #11 or #15 blade
- Trocars/ports
- Blunt or nontraumatic graspers
- Maryland and right-angle dissectors
- Electrocautery hook
- Clip appliers
- Specimen retrieval bag
- Insufflation needle and gas tubing
- Laparoscopic irrigator with sterile saline
- Laparoscopic scissors and endoscopic peanuts
- Radiopaque gauze sponges (4x4 or 8x4)
- Closing device
- Grounding pad
- If cholangiogram: C-arm drape, cholangiogram catheter, contrast dye
Be prepared in the event the surgeon needs to convert the laparoscopic cholecystectomy to an open or abdominal cholecystectomy.
- General instruments and a retractor set should be available, along with laparotomy sponges, dissector sponges (kittners/peanuts), an extended electrocautery tip, and additional suture of the surgeon’s choosing.

Suture
Absorbable suture of the surgeon’s choosing
Dressing
Skin adhesive, self-adhesive wound approximating strips, or adhesive bandages
Procedure
To perform this procedure, the surgeon will
- Once the ports are in place and the abdomen is sufficiently inflated, grasp the gallbladder through the medial port with blunt grasping forceps.
- Expose the Triangle of Calot (where the cystic duct and common hepatic duct form the common bile duct) using a grasper, endo-peanut, and/or energy device.
- Dissect the base of the gallbladder off the liver bed using an endoscopic dissector, hook, scissors, or energy device.
- Clip and divide he cystic artery and duct using a hemoclip, scissors, or energy device.
- Dissect the gallbladder off the liver using a hook or spatula.
- Place the gallbladder in the retrieval bag and remove it through a port.
- Irrigate the abdomen, if needed.
- Once hemostasis is achieved, turn the gas off, remove all trocars and instruments, and decompress the peritoneum of CO2
- Close the surgical wounds
- Use local anesthetic at the trocar sites (if it is the surgeon preference).
- Apply dressings.1,3
Possible Complications
- Visceral or vascular injury can occur with trocar placement
- CO2 gas may diffuse into the patient’s bloodstream, causing respiratory acidosis
- High pressure can cause bradycardia or gas embolus
- Bile leak or stones fall into the peritoneum
- Bile duct or other structure injury4,5
- Bleeding
Postoperative Recovery
- Patients may be placed in left side-lying Sim’s, semi-Fowler’s, or high Fowler’s position to allow for comfort and facilitate movement of remaining CO2.3,5
- Most patients are discharged within four to eight hours following the procedure.
- Patient’s must be alert and oriented, be hemodynamically stable, tolerate oral fluids, and have voided on their own.3
Editor's note: This content is adapted from AORN eGuidelines+. If your facility subscribes to eGuidelines+, you can access the full content.
References:
- Neil JA. Surgery of the liver, biliary tract, pancreas, and spleen. In: Rothrock JC, McEwen DR, eds. Alexander’s Care of the Patient in Surgery. 15th ed. St. Louis, MO: Elsevier Mosby; 2015:350-382.
- Guidelines for the clinical application of laparoscopic biliary tract surgery. Society of American Gastrointestinal and Endoscopic Surgeons. Accessed January 24, 2023. http://www.sages.org/publications/guidelines/guidelines-for-the-clinical-application-of-laparoscopic-biliary-tract-surgery/.
- Thomas BR. Cholecystectomy: take a look at two options. Nursing. 2009;39(2):36-39.
- Brenner P, Kautz DD. Postoperative care of patients undergoing same-day laparoscopic cholecystectomy. AORN J. 2015;102(1):16-29.
- Beckingham IJ. ABC of diseases of liver, pancreas, and biliary system. Gallstone disease. BMJ. 2001:322:91-94
AORN Resources
AORN members can access:
If your facility subscribes to eGuidelines+, you can access:
- Instruments at a Glance | AORN eGuidelines+
- Positioning at a Glance | AORN eGuidelines+
- Procedures at a Glance | AORN eGuidelines+
- Room Setup at a Glance | AORN eGuidelines+
- Skin Prep at a Glance | AORN eGuidelines+
- Patient Skin Antisepsis Guideline| AORN eGuidelines+
- Positioning the Patient Guideline | AORN eGuidelines+

