Facial Prep
By: Adapted from eGuidelines+ by Rachelle Williams MSN, RN, CNOR
Published: 11/14/2023
Before Prepping
Before the patient enters the OR, confirm what prep agent will be used; this will allow you to verify with the patient any allergies, assess for any open areas near the incision site (which may contraindicate an agent’s use), and verify that the prep agent’s manufacturer’s instructions for use (IFU) indicates that the agent can be used near the eyes, nose, and mouth.1-3 Different resources may be used to confirm the antiseptic agent to be used, such as the surgical preference card or preoperative huddle led by the surgeon.
The following preps are contraindicated for use on the face:
- 4% chlorhexidine gluconate4,5
- 2% chlorhexidine gluconate with alcohol and iodine povacrylex with alcohol; if these agents encounter hair, it can take up to one hour to dry; the patient cannot be draped until the prep solution has completely dried.6,7
- Povidone-iodine8 and chloroxylenol can be used on the face; however, they are contraindicated for use in the eye and if the patient is allergic to the solution.8,9
Regardless of what antiseptic agent you will be using, prepare the supplies ahead of time and follow these steps:
- Perform hand hygiene according to your site-specific policy.
- Prepare the material for the sterile set-up that will be opened onto a prep stand; if a sterile prep kit is not used, the contents opened could include a small basin(s), sponge sticks, and 4 x 4 sterile radiopaque sponges.
- Expose the area to be prepped; if needed, use a rubber band (a band without a metal piece) to secure hair away from the prepped area.
- While a nonsterile person holds the patient’s head slightly off the table, place a fluid-resistant prep pad under the patient’s head and place towels around the face to prevent pooling of the solution;2 remove them after the prep is completed. For a facial prep, place a cotton ball into the patient’s ear to prevent pooling of the solution into the ear canal; remove it after the prep is completed. For an ear prep, place a sterile cotton ball into the patient’s ear to prevent pooling of the solution into the ear canal; a member of the sterile team should remove the cotton ball with a sterile instrument after the prep has dried and before the drape has been applied.
- Lubricate and protect the patient’s eyes from the prepping solution; the method will depend on your site-specific policy. (This task may be performed by an anesthesia team member.)
- Ensure that the prepped area is large enough to allow for drape shifting, extension of the surgical incision (eg, additional tissue when checking margins for suspected malignant areas on the face), potential drain sites, or additional incisions.2,3
- Don sterile gloves before starting the prep (nonscrubbed team members).2,3
Prepping with Povidone-Iodine Paint
When prepping with povidone-iodine paint:
- Use a sterile applicator saturated with the paint solution to paint the area being prepped, beginning at the operative site and moving outward to the periphery.2,3
- Discard the applicator after reaching the periphery.2
- Use a new sterile applicator saturated with the paint solution and repeat steps 1 and 2 as many times as necessary to achieve complete coverage and comply with facility protocol and the manufacturer’s IFU.3
- Allow the paint solution to dry completely3 (eg, minimum of two minutes).8
Povidone-iodine paint should be used with caution for patients who are susceptible to iodism (eg, patients with burns or thyroid disorders, pregnant women).3 Iodophors can cause skin irritation with prolonged contact and can be absorbed by mucous membranes.3 An allergy to seafood does not indicate an allergy to iodine.2,3
Prepping with Chloroxylenol 3%
When prepping with chloroxylenol 3%, follow steps 1 to 4 in the “Prepping with Povidone-Iodine Paint” section. Unlike povidone-iodine paint, chloroxylenol 3% can be left to dry or blotted off with a sterile towel.
Types of Facial Preps
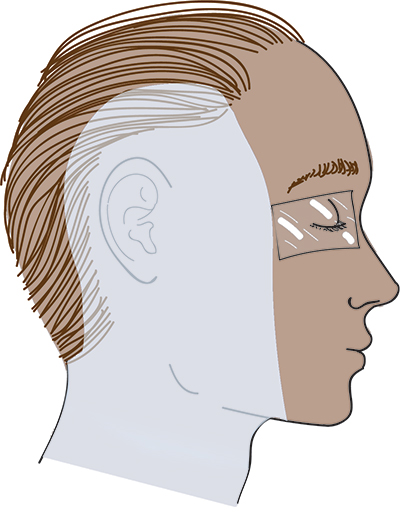
Facial preps can be used for procedures of the face, nose, ears, and oral area:
- For a procedure on the face (eg, removal of a facial lesion), begin prepping at the incision site and work your way away (clean to dirty), ensuring that the prep extends beyond the surgical margins. (If the surgical site is near the eyes, refer to the Skin Prep at a Glance: Eye on AORN eGuidelines+, which you can access if your facility has a subscription to eGuidelines+.)
- For a nasal procedure, prep the external nose (including the nostrils) and the surrounding area of the face, extending the prep toward the hairline, the shoulders, and down to below the jawline. (Usually, the internal nose is not prepped.)10
- For an oral procedure, prep the external area around the mouth and surrounding face, and possibly the oral cavity, depending on the specific procedure being performed and your facility policy.11
- If the oral cavity is being prepped, take care to prevent aspiration of the antiseptic solution (eg, use a throat pack).2
- Tonsillectomy and adenoidectomy procedures are considered “clean” procedures, which means that they are not sterile procedures, and no skin prep is used.10

- For an ear procedure, begin prepping the auricle (also known as pinna or external ear), working outward to include the periauricular area behind the ear.10 The prep will extend to hairline, the shoulders, and beyond midline of the face and to the jawline.10
Special Considerations
- Patients who will be having surgery of the head or face should shampoo their hair before surgery.2
- Before prepping, isolate nonintact skin that is not part of the procedure with a sterile barrier drape.2
- If the incision site is the most contaminated part of the area to be prepped (eg, open wound), prep the area with the lower bacterial count first, before prepping the area with a higher contamination.2
- It is important to use caution on fragile skin, such as burns, open wounds, or malignant areas.2
- After the procedure, the antiseptic should be removed from the patient’s skin, unless otherwise indicated by the manufacturers IFU.2
Editor's note: This content is adapted from AORN eGuidelines+. If your facility subscribes to eGuidelines+, you can access the full content. This article is intended to serve as a guide to prepping and may not represent every available antiseptic solution. Always prep in accordance with the manufacturer’s instructions for use for the antiseptic solution being used. AORN does not endorse any commercial company’s products or services, including particular skin preparation products. Inclusion of a solution in this article does not constitute an endorsement by AORN of the quality or value of such solution or process, or of the claims made by its manufacturer.
References
- Guideline Essentials Quick View: Patient Skin Antisepsis. AORN. Accessed February 24, 2023. https://www.aorn.org/guidelines-resources/guidelines-for-perioperative-practice/guideline-essentials
- Guideline for preoperative patient skin antisepsis. In: Guidelines for Perioperative Practice. Denver, CO: AORN, Inc; 2022:623-680.
- AORN. Preoperative Skin Antisepsis [DVD]. Woodbury, CT: CineMed, Inc; 2015.
- LABEL: HIBICLENS – chlorhexidine gluconate solution. DailyMed. December 21, 2021. Accessed May 4, 2023. https://dailymed.nlm.nih.gov/dailymed/drugInfo.cfm?setid=8b37a721-79bb-4051-95a7-fcb4edebfcb7
- Antiseptic skin cleanser (chlorhexidine gluconate 4% solution). DailyMed. Revised December 2012. Accessed May 4, 2023. https://dailymed.nlm.nih.gov/dailymed/fda/fdaDrugXsl.cfm?setid=76cfedb3-25ed-4c12-8ebc-b57f029fedaa&type=display
- ChloraPrep One-Step/ChloraPrep with Tint. BD. Accessed May 4, 2023. http://www.bd.com/Documents/labels/IP_ChloraPrep-10-5mL-Clear_PL.pdf
- 3M DuraPrep surgical solution: patient preoperative skin preparation. 3M. September 29, 2006. Accessed May 4, 2023. http://multimedia.3m.com/mws/media/429254O/duraprep-patient-preoperative-skin-preparation.pdf
- Scrub Care povidone iodine topical paint. DailyMed. November 22, 2022. Accessed May 4, 2023. https://dailymed.nlm.nih.gov/dailymed/drugInfo.cfm?setid=fbe92fa9-273c-45be-a46d-437587507bee
- Zinn J, Jenkins JB, Swofford V, Harrelson B, McCarter S. Intraoperative patient skin prep agents: is there a difference? AORN J. 2010; 92(6):662-674. https://doi.org/10.1016/j.aorn.2010.07.016
- Goldmen Maxine A. Otorhinolaryngologic (ENT) surgery. In: Pocket Guide to the Operating Room. 4th ed. Philadelphia, PA: F.A. Davis; 2020:819-902.
- Derose TJ. Otorhinolaryngologic surgery. In: Rothrock JC, ed. Alexander’s Care of the Patient in Surgery. 15th ed. St Louis, MO: Elsevier Mosby; 2015:626-678.
AORN Resources
AORN members can access:
- Patient Skin Antisepsis Guideline Essentials - AORN
- Back to Basics 2.0: Preoperative Patient Skin Antisepsis - AORN Journal
- Guideline Quick View: Patient Skin Antisepsis - AORN Journal
- Key steps to prepare for preoperative patient skin antisepsis - AORN Journal
- Reducing the Risk of Surgical Site Infection With Effective Preoperative Patient Skin Antisepsis - AORN Journal

