Abdominal Skin Prep
By: Adapted from eGuidelines+ by Rachelle Williams MSN, RN, CNOR
Published: 9/11/2023
Before Prepping
Before the patient enters the OR, confirm what prepping agent will be used; this will allow you to verify with the patient any allergies and assess for any open areas near the incision site, which may contraindicate an agent’s use. Different resources may be used confirm the antiseptic agent to be used, such as the surgical preference card or preoperative huddle led by the surgeon. The manufacturer's instructions for use (IFU) for the antiseptic agent provides information that may affect application, including sites on which and patients in whom it should not be used or be used with caution.
The skin prep occurs before the surgical incision, but after the patient has been positioned. For abdominal procedures, the patient is positioned in supine or a modification of supine. Regardless of what antiseptic agent you will be using, prepare the supplies ahead of time and follow these steps:
- Perform hand hygiene according to your site-specific policy.
- Expose the area to be prepped (the abdomen).
- Ensure that the prepped area is large enough to allow for drape shifting, extension of the surgical incision, potential drain sites, or additional incisions.
- Apply pooling towels on each side of the patient to ensure that prep does not accumulate underneath the patient.1
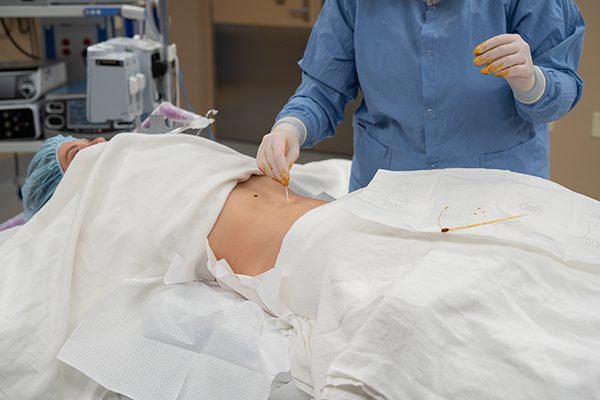
- Use cotton-tipped applicators moistened with prep solution to clean the umbilicus, removing any debris.1,2
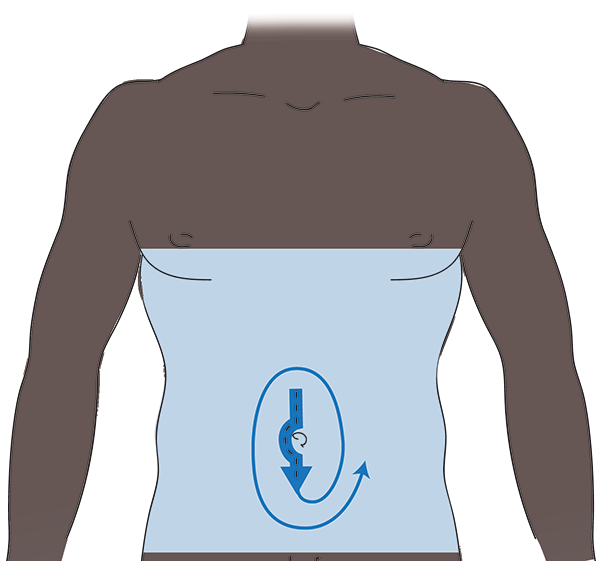
- Prep from the nipple line to midthighs.
It is recommended that a nonscrubbed team member apply the antiseptic using aseptic technique;1,2 if you are not performing the prep, it is your responsibility as the patient advocate to ensure that the prep is being applied according to the manufacturer’s IFU using aseptic technique.
Alcohol-Based Antiseptics
Alcohol-based antiseptics are considered superior in terms of clinical and antimicrobial effectiveness than other no-alcohol antiseptics.3 If an alcohol-based prep is used, it is imperative that you include it in your fire risk assessment calculation and follow the IFU for the dry time (eg, three minutes on hairless skin and up to one hour for hair).
There are two types of alcohol-based antiseptics: 2% chlorhexidine gluconate (CHG) with alcohol and iodine povacrylex with alcohol. The prefilled sterile applicators come in different sizes that contain a glass ampule of the prep solution. It is important that you choose the correct size according to the IFU for the surgical site area you are prepping (Table 1).4,5 Before starting the prep, you will need to activate the applicator. It is recommended that you let the solution flow freely (no shaking) to the applicator sponge. If you are using an applicator that is long enough to avoid contact with the gloved hand, antiseptic, and patient’s skin, you can don nonsterile gloves. If there is a potential risk for contamination, you should don sterile gloves.1,2
Table 1. Applicator sizes and prep areas for 2% CHG with alcohol and iodine povacrylex with alcohol
Solution | Applicator size | Prep area |
2% CHG with alcohol | 26 mL | 13.3 in x 13.2 in |
10.5 mL | 8.4 in x 8.4 in | |
3 mL | 4 in x 5in | |
1 mL | 2.5 in x 2.5 in | |
Iodine povacrylex with alcohol | 26 mL | 15 in x 30 in |
After the procedure, the prep should remain on the patient to provide continued antimicrobial activity. This should be discussed with the patient and their family preoperatively, so they are not surprised when they see the prep on the patient’s skin.
Prepping with 2% CHG with Alcohol
The CHG prep comes in two different tints: orange and teal. The orange tint is more visible on fair skin tones whereas the teal tint is more visible on medium to dark skin pigmentation.6 To prep with 2% CHG with alcohol:
- Use the prefilled applicator to apply the solution, starting at the incision site using gentle back-and-forth strokes following the manufacturer’s IFU (eg, 30 seconds) and then proceed to the periphery (ie, clean to dirty).1,2
- If there is pooling of the solution at the umbilicus, use a sterile 4 x 4 gauze pad to wick (soak up) the pooled solution.
- Remove the pooling towels without touching any of the prepped skin.
- Check the bed to ensure that there is no prep solution on the sheets; if there is, remove the linen under the patient.
Prepping with Iodine Povacrylex with Alcohol
When prepping with iodine povacrylex with alcohol, perform the steps listed for 2% CHG with alcohol, but do not use a back-and-forth motion. Instead, paint the prep on, which means that you move from clean to dirty without going over an already prepped area.7
Alternative Agents
Alternatives to alcohol-based antiseptics, if not contraindicated, include 4% CHG, povidone-iodine scrub and paint, and chloroxylenol 3% (PCMX).8 These agents do not come in a prefilled applicator. They require a sterile set-up opened on a prep stand. The contents opened could include a small basin(s), sponge sticks, and 4 x 4 gauze (some sites will only use 4 x 4 sterile radiopaque sponges or a premade kit with foam sponges).
After performing hand hygiene:
- Don sterile gloves (nonscrubbed team members).
- Place sterile pooling towels on the sides of the patient.
- Apply the antiseptic using aseptic technique.
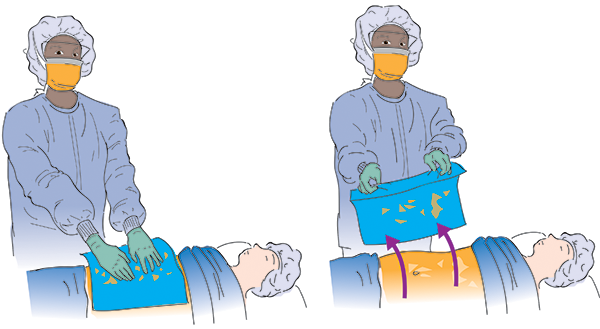
- Use a sterile towel to blot the prepped area.
- Remove the pooling towels.1,2
It should be noted that these agents will get wiped off the patient after the procedure.
Prepping with 4% CHG
When prepping with 4% CHG,
- Use a sterile sponge stick with sterile gauze or a foam sponge to apply the antiseptic, starting at the incision site and moving outward to the periphery (ie, clean to dirty).1,2
- Discard after reaching the periphery and use a new sponge stick with new gauze or a new foam sponge and repeat the process until you have achieved complete coverage and complied with the manufacturer’s IFU for application time (eg, minimum of two minutes).9,10
- While avoiding contact with unsterile items, place a sterile towel over the prepped area to blot the scrub solution on the prepped site.8
- Remove the towel by grasping the far end of the cuffed towel and pulling it toward you.1
- Repeat the steps one more time and then remove the pooling towels.
Prepping with Povidone-Iodine Scrub and Paint
When prepping with povidone-iodine scrub and paint,
- Start with the iodine scrub and use a sterile applicator (eg, foam sponge) to scrub the abdomen from the incision site outward to the periphery.
- After repeating the process (eg, five minutes according to the IFU),11,12 use a sterile towel to blot the prepped area to remove the scrub solution.
- Apply the iodine paint by painting the solution from clean to dirty and not going over an already prepped area; you will do this twice with two separate sterile applicators.
- Allow the paint solution to dry1,13 according to the IFU (eg, two minutes);14 do not use a towel to blot the prepped area.
Prepping with Chloroxylenol 3%
This antiseptic can be applied the same as 4% CHG; however, it could be left to dry or blotted with a sterile towel.
Special Considerations
If a patient has a stoma near the incision site, prep the area with the lower bacterial count first and then the site with the higher count.
Editor's note: This content is adapted from AORN eGuidelines+. If your facility subscribes to eGuidelines+, you can access the full content. This article is intended to serve as a guide to prepping and may not represent every available antiseptic solution. Always prep in accordance with the manufacturer’s instructions for use for the antiseptic solution being used. AORN does not endorse any commercial company’s products or services, including particular skin preparation products. Inclusion of a solution in this article does not constitute an endorsement by AORN of the quality or value of such solution or process, or of the claims made by its manufacturer.
References:
- Preoperative Skin Antisepsis [DVD]. Woodbury, CT: CineMed, Inc; 2015.
- Guideline for preoperative patient skin antisepsis. In: Guidelines for Perioperative Practice. Denver, CO: AORN, Inc; 2022. In press.
- Allegranzi B, Bischoff P, de Jonge S, et al. New WHO recommendations on preoperative measures for surgical site infection prevention: an evidence-based global perspective. Lancet Infect Dis. 2016;16(12):e276-e287. https://doi.org/10.1016/S1473-3099(16)30398
- BD ChloraPre Preoperative antiseptic skin preparation with sterile solution. Accessed May 25, 2023. https://www.bd.com/en-ca/offerings/capabilities/infection-prevention/skin-preparation/bd-chloraprep-patient-preoperative-skin-preparation-products/bd-chloraprep-applicators.
- Duraprep surgical prepping solution. 3M. Accessed May 25, 2023. https://www.3m.com/3M/en_US/p/d/v000190116/
- McDaniel CM. Visibility of tinted chlorhexidine gluconate skin preparation on varied skin pigmentations. 2017;40(1):e44-e48. https://doi.org/10.3928/01477447-20160926-01
- 3M DuraPrep surgical solution: patient preoperative skin preparation. 3M. http://multimedia.3m.com/mws/ media/429254O/duraprep-patient-preoperative-skin-preparation.pdf. Published September 29, 2006. Accessed February 15, 2023.
- Zinn J, Jenkins JB, Swofford V, Harrelson B, McCarter S. Intraoperative patient skin prep agents: is there a difference? AORN J. 2010;92(6):662–674. https://doi.org/10.1016/j.aorn.2010.07.016.
- HIBICLENS – chlorhexidine gluconate solution. DailyMed. https://dailymed.nlm.nih.gov/dailymed/drugInfo. cfm?setid=8b37a721-79bb-4051-95a7-fcb4edebfcb7. Updated December 21, 2021. Accessed February 15, 2023.
- Antiseptic skin cleanser (chlorhexidine gluconate 4% solution). DailyMed. https://dailymed.nlm.nih.gov/dailymed/fda/fdaDrugXsl.cfm?setid=76cfedb3-25ed-4c12-8ebc-b57f029fedaa. Revised December 2012. Accessed February 15, 2023.
- Betadine surgical scrub. Betadine. https://betadine.com/medical-professionals/betadine-surgical-scrub/. Accessed March 12, 2021.
- Scrub Care povidone iodine cleansing scrub. DailyMed. https://dailymed.nlm.nih.gov/dailymed/drugInfo. cfm?setid=19182492-4cde-481f-bac0-7b47ac8cad4e. Updated November 17, 2022. Accessed February 15, 2023.
- Betadine solution. Betadine. https://betadine.com/medical-professionals/betadine-solution/. Accessed February 15, 2023.
- Scrub Care povidone iodine topical paint. DailyMed. https://dailymed.nlm.nih.gov/dailymed/drugInfo. cfm?setid=fbe92fa9-273c-45be-a46d-437587507bee. Updated November 22, 2022. Accessed February 15, 2023.
AORN Resources
AORN members can access:
- Patient Skin Antisepsis | AORN Guideline Essentials
- Preoperative Patient Skin Antisepsis | AORN FAQS
- Back to Basics 2.0: Preoperative Patient Skin Antisepsis - AORN Journal
- Guideline Quick View: Patient Skin Antisepsis - AORN Journal
- Key steps to prepare for preoperative patient skin antisepsis - AORN Journal
- Reducing the Risk of Surgical Site Infection With Effective Preoperative Patient Skin Antisepsis - AORN Journal

