Focus on What’s Necessary at Year’s End
The holiday season can throw some employees off track, draining their levels of engagement and enthusiasm for their jobs at the end of a long year....
This website uses cookies. to enhance your browsing experience, serve personalized ads or content, and analyze our traffic. By clicking “Accept & Close”, you consent to our use of cookies. Read our Privacy Policy to learn more.
By: Carina Stanton | Contributing Editor
Published: 5/2/2024
While the research is mixed, the promise of AI-assisted colonoscopy includes a double-digit boost in adenoma detection rates (ADR). Two experienced gastroenterologists say the technology is worth the hype.
AI assistance should be used for colonoscopies now and for more GI procedures in the future, according to Ahmed Saeed, MD, of Premier Gastroenterology of Kansas City (Mo.) and Benjamin H. Levy III, MD, of University of Chicago Medicine. During colonoscopies, AI helps gastroenterologists identify difficult-to-see flat polyps and polyps hidden by folds.
“It’s well-documented that polyps can be missed during colonoscopy due to several reasons, including failure of recognition, particularly if the angle of view isn’t right or there is a reflection or other visual block,” says Dr. Saeed. “That’s where AI comes in. It assists with adenoma detection by highlighting polyp areas we couldn’t normally see with speed and accuracy.”
The literature regarding a collection of randomized controlled trials on the topic leans heavily in favor of AI-assisted colonoscopy leading to higher ADR. One 2021 review of six such trials, for example, found ADR was 33.7% with AI assistance and 22.9% without during colonoscopies. Favorable ADRs were also found in a separate 2021 review, although several of the studies reported false positives. A 2020 prospective crossover study found that the adenoma miss rate was 40% for traditional colonoscopies and only 14% for procedures assisted by AI. Polyps were missed 46% of the time without AI and only 13% of the time with it. The study also found that smaller adenomas measuring 5-10mm were missed less with the use of AI.
Data like these led Dr. Saeed to begin using AI technology in colonoscopy procedures when the technology first received FDA market approval in 2021. He notes that while AI doesn’t replace the skill of the gastroenterologist and GI team, it can serve as a valuable adjunct to increase their ADR. “AI-assisted colonoscopy can be especially helpful for endoscopists who have lower ADRs to increase them, especially among less experienced gastroenterologists,” says Dr. Levy, who believes the technology should be used for most patients, not just high-risk ones. “It’s really amazing technology that gives us that extra visibility to make sure no lesions are missed.”
Adopting AI-assisted technology is a process that’s as simple as flipping a switch, say Drs. Saeed and Levy. A box is added to the endoscope’s light source. Once connected, the AI functionality highlights areas on the screen where a suspected polyp is and makes an optional sound alert. “It’s the physician’s responsibility to evaluate the area it highlights and confirm it’s a polyp that needs to be removed,” says Dr. Saeed. In his experience, the alerts are highly accurate.
Dr. Levy finds AI-assisted technology helpful to identify areas that aren’t as simple to visualize, such as when there is residual stool in the colon or when the polyp is flat or located in folds. AI also enhances visualization during the scope withdrawal process when insufflation and the position of the scope can sometimes impact the view.
“Any tool we have at our disposal to improve colonoscopy should be something we have in our arsenal for our patients,” says Dr. Levy. The doctors say minimal team training is required to begin using AI-assisted technology in the quest to detect and remove colon cancer. The technology includes periodic software updates, which Dr. Levy likens to a smartphone update. “Teams should collaborate and be educated on any changes the update brings, but the actual updating is seamless,” he says.
As a gastroenterologist and a cellist, University of Chicago Medicine’s Benjamin H. Levy III, MD, uses music to spread awareness about health. Possessing a professional music background that includes a Fulbright Fellowship in Paris, Dr. Levy has leveraged his place in the music world to make colon cancer screening more approachable and mainstream.
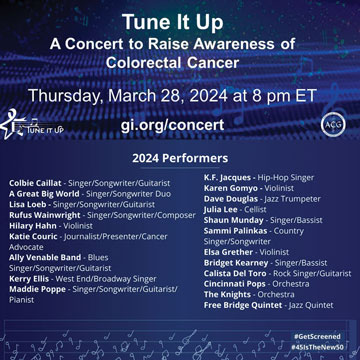
His latest musical project, “Tune It Up: A Concert to Raise Colon Cancer Awareness,” is sponsored by the American College of Gastroenterology. It debuted in March and can be viewed for free at gi.org/concert.
Now in its fourth year, the Tune It Up concert brings top performers in classical, country, rap and other genres together for a good cause. This year’s show features Rufus Wainwright, Colbie Caillat, A Great Big World and Lisa Loeb, some of whom shared their own connections to colon cancer. Dr. Levy played cello in his group of gastroenterologist colleagues and other musicians called The Beacons.
“For me, music inspires health,” he says. “We hope GI practices across the country will promote free year-round access to the concert to capture a wider audience and to encourage colon cancer screening starting at age 45.”
—Carina Stanton
Dr. Saeed makes it a point to describe to his patients the role that AI plays in their colonoscopies. “I try to simplify by letting them know that AI offers another very accurate set of eyes to help identify any precancerous lesions in the colon,” he says.
With patients playing the role of healthcare consumers when trying to decide where to get their colonoscopies, Dr. Levy believes centers that offer and promote AI-assisted colonoscopy will gain a competitive edge.
That’s especially important because the market for colonoscopies has expanded with the new recommended age for a patient’s first colonoscopy lowered to 45. If no polyps are found, patients can wait 10 years until their next screening.
“We don’t know when someone will get their next colonoscopy, so it’s critical we don’t miss anything,” says Dr. Levy. “Giving them a colonoscopy that is as accurate as possible, especially for smaller polyps, gives us one more way to prevent colorectal cancer.” AI, he says, boosts that accuracy.

The AI technology these doctors use costs about $60,000 to purchase, or it can be leased on a subscription basis for about $1,000 per month. Dr. Saeed notes that AI is not reimbursable per colonoscopy because there isn’t a CPT code assigned for it yet, but he considers the extra expense worthwhile because he believes it enables a higher-quality procedure.
The technology’s compatibility with any major brand of colonoscope makes it a versatile purchase for the long term, says Dr. Levy, who predicts its cost will decline as more gastroenterologists bring AI into their practices.
While AI in the GI space is most commonly used in colonoscopy, Dr. Saeed says its applications will soon include assistance with the detection of dysplasia in Barrett’s esophagus and the ability to determine what type of polyps are detected and how likely they are to be malignant.
“These advances are all very exciting as we look to the short- and long-term impacts of AI to improve GI practice,” says Dr. Levy. “Much like how the iPhone changed our lives, AI technology in GI care is revolutionizing our practice and will hopefully become as ubiquitous as the iPhone so we can save more lives.” OSM
The holiday season can throw some employees off track, draining their levels of engagement and enthusiasm for their jobs at the end of a long year....
While this year’s celebration of America’s nearly 74,000 Certified Registered Nurse Anesthetists (CRNAs) and residents in nurse anesthesiology programs technically runs...
The Association of periOperative Registered Nurses (AORN) is pleased to announce the appointment of David Wyatt, PhD, RN, NEA-BC, CNOR, FAORN, FAAN, as its new Chief Executive Officer...