- Home
- Article
The Dos and Don’ts of Establishing a Culture of Safety
By: Danielle Bouchat-Friedman | Senior Editor
Published: 10/19/2023
Here’s how to make systematic changes that are crucial in the highly scrutinized outpatient environment.
Making improvements to your facility’s safety culture is no easy task. While healthcare staff work hard to provide the best care for their patients, safety continues to be a concern. Around one in 20 U.S. patients experience preventable harm events during their care, and healthcare facilities have the highest rates of occupational injury and illnesses among all workplaces.
Mairin Monteath, BA, program officer, education and advocacy for Staff and Patient Safety, an organization dedicated to advocating for the physical and psychological safety of staff and patients in health care, and Chamindika Konara, PhD, a contributor to the organization, share their tips on how healthcare facilities can create sustainable change, both big and small, that will last well beyond initial implementations.
• DO discuss common barriers to change and how staff can overcome them. There are several recognized barriers to effective change, both on the individual and the organizational level. “One of the most common barriers that leaders will face is resistance to change,” says Ms. Monteath. “It’s natural for us to want to stay in our comfort zone of what we have been taught before, and what we are used to doing. In health care, there’s an additional concern for patient care, which can lead to staff being hesitant to change the practices that they are accustomed to,” she says.
Dr. Konara says empowering staff at each stage of change implementation is vital to overcoming this barrier. “When clinical teams understand why the change is necessary and feel as though they are involved in the process, they are significantly more likely to enact the change in practice and encourage others to do so,” she says.
When clinical teams understand why the change is necessary and feel as though they are involved in the process, they are significantly more likely to enact the change in practice and encourage others to do so.
Chamindika Konara, PhD
• DON’T be discouraged by staff who are stuck in their ways. Changing a practice that is so ingrained into the day-to-day, like removing scalpel blades, does require some convincing for more-experienced nurses who are used to their methods. Ms. Monteath believes there can be a tendency to feel as though those who resist change are the enemy standing in the way of achieving the goals, but that’s a misconception. “When change is communicated effectively and change champions engage with those resisting, we’ve seen that initially resistant staff members turn into some of the biggest advocates,” she says. “Our advice for when nurses share their resistance is to listen carefully, and not dismiss their concerns. Feedback is important for process improvement, and learning from those who ask questions will only better the implementation. The most successful change projects we’ve seen are those that engage with all stakeholders in the change planning, execution and feedback processes.”
The worst thing that can happen is that stakeholders don’t care. No change is perfect, notes Dr. Konara, and any concerns that can’t be immediately addressed should be recorded and evaluated for future improvements.
• DO foster open communication. Ms. Monteath and Dr. Konara have found healthcare facilities that make time for open communication have the most success. “Embedding time for questions during regular communication processes, such as safety huddles, time outs or staff surveys, is an easy way to demonstrate a commitment to open communication,” says Dr. Konara. “While these activities may take time and effort, we have seen that the investment has resulted in a positive ROI, which is supported by a vast body of evidence.”
Running “good-catch campaigns” is an excellent example of something that leaders can implement to encourage staff to speak up for safety, says Ms. Monteath. “Some facilities have implemented emails to highlight good catches, with regular awards to celebrate the staff who have made a report. Good-catch campaigns build rapport within healthcare teams and provide strong incentives for action to be taken to improve safety,” she says. How leaders respond to staff speaking up is just as vital. “If staff have leaders who ignore their concerns or slight them for speaking up, they are unlikely to communicate openly again,” says Ms. Monteath.
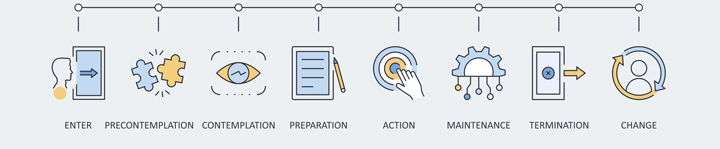
Kotter’s 8-Step Process for Leading Change is a process developed by John P. Kotter, a Harvard Business School professor. He designed the model to help leaders successfully implement organizational change. It is particularly helpful for complex settings like health care, as it considers how to work with multiple stakeholders and prioritizes direct engagement from those who will need to enact the change. Mairin Monteath, BA, program officer, education and advocacy for Staff and Patient Safety, an organization dedicated to advocating for the physical and psychological safety of staff and patients in healthcare, and Chamindika Konara, PhD, a contributor to the organization, break down the eight steps.
• Create a sense of urgency. Change champions need to help clinical teams understand why the change is necessary, and to encourage their participation in the change process. If facilities are implementing a new product, change champions can build excitement in this stage by involving frontline clinicians in product evaluations.
• Build a guiding coalition. In addition to the change champion, the guiding coalition may include internal mini-champions from within the clinical teams to help support training needs, and external support such as product sales representatives or subject matter experts.
• Develop the vision and strategic plan. A clear vision for the change, such as compliance with updated infection guidelines, will help to keep teams focused during implementation. This is also the time to plan out the strategy for implementation, such as training days.
• Communicate the change. Healthcare facilities should leverage all of their communication channels, including protected learning time, email and even breakroom chats. Education and open-ended discussions are highly effective ways that facilities and change champions can counter resistance.
• Empower actions for change. Successful change projects require organizational persistence of key messaging and adequate support through resources. For product implementation, consider running multiple training sessions to help build your clinical team’s confidence.
• Accomplish short-term wins. Healthcare facilities should break down their implementation project into smaller, achievable goals. Then, acknowledge those stakeholders who complete them. Some examples include providing certificates for those who complete training, coordinating staged usage goals and setting incremental improvement goals.
• Build on the change. Evaluate progress and identify what is going well and any areas for improvement. It’s vital for change champions to encourage feedback from all stakeholders so they can make relevant adjustments to the implementation plan.
• Make change stick. One of the best ways to ensure permanent change is by finding ways to build it into systems. Systematic changes aren’t reliant on human factors and help prevent old habits from slipping in when things get busy or new staff join the team.
— Mairin Monteath, BA and Chamindika Konara, PhD
• DON’T take early victory laps. Ms. Monteath and Dr. Konara believe that many change projects fail because victory is declared too early, and the timelines are often underestimated. “What we found effective is aiming for small goals over a long period of time, with the understanding that sustainable change that sticks takes time,” says Dr. Konara. “Successful change requires organizational persistence, and a commitment at all levels to ensure that long-term improvements can be maintained.
“Change is not a stagnant endpoint, but a continuous process toward incremental improvements and milestones. This is why it’s also important to evaluate the change project during the process and communicate these results with the rest of the teams,” she says.
Creating the right climate
Healthcare settings, regardless of their size, are complex environments with multiple stakeholders and competing demands for time and attention, note Ms. Monteath and Dr. Konara. “We can’t forget that the patient needs to remain at the center of practice, and that what we do in outpatient settings affects people’s lives,” says Dr. Konara. She says that outpatient settings can often adopt safety improvements more quickly and more cost-effectively than large hospitals, because they can be more agile and often deal with less red tape. In the end, the most successful changes are systematic ones, where all stakeholders understand the reasons behind the moves and feel empowered by them. Changes that stick need time, so focus on the improvements that have been made while looking forward to what else can be done. OSM
.svg?sfvrsn=be606e78_3)
.svg?sfvrsn=56b2f850_5)