Focus on What’s Necessary at Year’s End
The holiday season can throw some employees off track, draining their levels of engagement and enthusiasm for their jobs at the end of a long year....
This website uses cookies. to enhance your browsing experience, serve personalized ads or content, and analyze our traffic. By clicking “Accept & Close”, you consent to our use of cookies. Read our Privacy Policy to learn more.
By: Jared Bilski | Editor-in-Chief
Published: 9/4/2024
When the former nurse manager of Kaiser Sacramento (Calif.) Ambulatory Surgery Center discovered potential issues with the information staff delivered to patients during the discharge process, it set off a chain reaction that led to major process changes, ambitious improvement goals and a place in the September issue of Outpatient Surgery Magazine as the winner of the 2024 OR Excellence Award for Patient Satisfaction & Experience.
Kaiser Sacramento is thriving today, but that wasn’t the case in the first quarter of 2023, when the center was ranked 27th out of the 29 Kaiser facilities based on its Care Experience Score of 71.6%, which was well below the 79.9% average score for the group. For Kaiser staff, this Care Experience Score is much more than just a benchmarking tool; it’s an integral part of Kaiser’s patient-care philosophy. “Care metrics are critical to the staff,” says Ericka F. Osborn, RN, BSN, nurse manager at Kaiser Sacramento. “In our moment we have with patients, we need to find out how they are — anxious, scared, uncomfortable? — and exactly what we can do on our side to make them feel more at ease.”
Care metrics give staff the insight they need to give patients the best possible experience. That’s why when Kaiser Sacramento saw its scores slipping, it sounded the alarm.
Based on responses in the center’s detailed Top Box scoring system — a systemwide patient survey platform that allows Kaiser facilities to receive third-party scoring on the patient experience through unbiased questions — leaders were able to dig in and find out where the problems were occurring.
“Our scores were showing that the recovery process was faltering, that patients weren’t getting good instructions,” says Ms. Osborn. Specifically, the instructions regarding recovery and home care were triggering the low scores. Kaiser’s gap analysis discovered that a protocol instituted during the pandemic — not having a family member at the bedside — was part of the problem and led to patient’s not fully understanding discharge instructions.
Sleepy, disoriented post-op patients claimed no one had spoken to them, and were confused about the term “home care.” Patients also claimed that they were only asked about their current status, not their overall experience, during post-op phone calls.
“We weren’t sure whether patients were forgetting the discharge info they received because they had just come out of anesthesia or they simply weren’t getting it,” says Ms. Osborn. “Regardless of the reason, we knew we had to change the outcome.”
Armed with an array of data on what needed to improve, Kaiser Sacramento put together a multipronged approach to do it — and it set an ambitious improvement goal. “We challenged ourselves to increase member care experience scores by at least 10% between the first quarter of 2023 through the first quarter of 2024 by adding caring moments from the start of contact until the day after their visit,” says Ms. Osborn.
Karen P. Valerie, RN, BSN, MSN, ASC director at NYU Langone Hospital-Long Island, knew the breakneck pace of the ASC setting — an environment where staff often have only small windows to interact with individuals undergoing surgery — often forced well-meaning providers to focus on a task, rather than the patient’s unique emotional needs. But she and her team were determined to find a better way to connect with patients in real time.
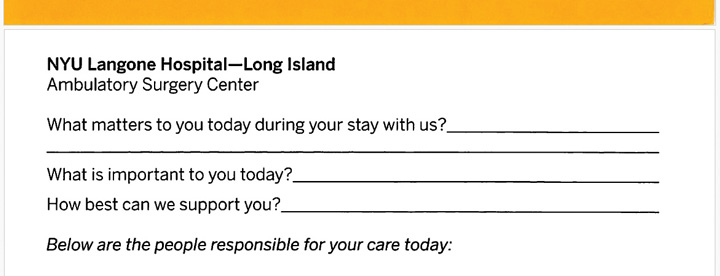
What they came up with was nothing short of brilliant in its simplicity. The center’s director, nurse manager and staff met to draft a welcome card patients would fill out while they wait for surgery or when the nurses begin the preparation for their surgery. To understand and meet patients’ needs, the cards ask them: What matters to you today during your stay with us? What is important to you today? and How can we best support you?
The wording of those three questions, says Ms. Valerie, was carefully selected so that patients will tell staff exactly what they need, whatever is bothering them, etc. The cards are collected and reviewed to meet the individual needs of each patient, and each nurse then communicates those needs during the handoff report. The benefits of these cards were immediately apparent, as facility rating scores increased. Best of all, the questions improved and deepened the provider-patient connection. “In surgery, we only have a few minutes to connect, and it’s very important to get to know the emotional needs of the patients,” says Ms. Valerie. “We try to do that here. When you bring down the patient’s anxiety and meet their needs at the point of service, it improves and optimizes everything about the patient outcome.”
—Jared Bilski
The action plan to achieve that double-digit lift included a strategic year-long project that emphasized engaging stakeholders, providing ongoing training via workshops and seminars related to patient-centered care and communication, and rolling out employee recognition programs to reward those who consistently provide exceptional care.
Some of the specific changes related to the formerly problematic post-op process included beginning the discharge in pre-op before any sedating medications were given; using the word “recovery” instead of “discharge” when describing expectations and instructions to follow after surgery; and adding a cover page and a large, bright neon sticker stating “Recovery and Home Care Instructions” to the important discharge paperwork.
When the dust settled, the data confirmed that the multipronged plan had indeed succeeded. In January 2024, the Facility Rating score hit 86.9%, a 15.3% increase from the previous year and well above the 10% bump that was originally thought too ambitious. Even better: In February, the score hit an all-time high 92.5%. Are Ms. Osborn and her team proud of the progress they’ve made? Of course. Are they satisfied? Not a chance. “Our job is to keep the ‘Care Scores’ elevated,” says Ms. Osborn. “We’re constantly striving to do better. It’s going well right now, but we can always improve.” OSM

Virtually every surgery center’s patient satisfaction scores take a dip or miss the target for time to time. What matters is how centers respond.
For Emory Ambulatory Surgery Center at Spivey Station in Jonesboro, Ga., that response not only lifted those slightly off-target scores, but it also earned the center an Honorable Mention spot in this year’s OR Excellence Awards in the Patient Satisfaction & Experience Category. There wasn’t one narrow initiative Emory employed to change the tide. Rather, it was a barrage of patient-satisfying extras that hit the mark.
“To boost patient satisfaction scores, several strategies were adopted, starting with the distribution of Thank You cards by Front Desk Administrator Ann Dorsey and the regular posting and review of patient survey results by myself and Shift Nurse Manager Jana Yates,MSN, RN,” says Persila A. Bencomo, MSN-NI, RN, clinical nurse manager. “Additional measures included staff recognition through e-recognition points, patient comfort amenities (coffee, food delivery and blankets if they get cold), pre-op and follow-up calls by nurses, and direct engagement with patients to address any issues.” Whether it’s the PACU nurses’ check-up callbacks the day after surgery or the detailed explanation nurses offer patients about what to expect immediately following the pre-op handoff, it was the sum of these extra steps that proved much greater than any one patient-satisfier on its own.
Ms. Bencomo says the effort to improve patient satisfaction scores also led to enhanced patient engagement and communication, which in turn fostered stronger patient-staff relationships and improved trust and cooperation. But it also led to several indirect benefits, too. “Staff morale has increased significantly. Recognition and positive feedback served as strong motivators and boosted overall job satisfaction,” she says.
—Jared Bilski
The holiday season can throw some employees off track, draining their levels of engagement and enthusiasm for their jobs at the end of a long year....
While this year’s celebration of America’s nearly 74,000 Certified Registered Nurse Anesthetists (CRNAs) and residents in nurse anesthesiology programs technically runs...
The Association of periOperative Registered Nurses (AORN) is pleased to announce the appointment of David Wyatt, PhD, RN, NEA-BC, CNOR, FAORN, FAAN, as its new Chief Executive Officer...