Focus on What’s Necessary at Year’s End
The holiday season can throw some employees off track, draining their levels of engagement and enthusiasm for their jobs at the end of a long year....
This website uses cookies. to enhance your browsing experience, serve personalized ads or content, and analyze our traffic. By clicking “Accept & Close”, you consent to our use of cookies. Read our Privacy Policy to learn more.
By: Jared Bilski | Editor-in-Chief
Published: 9/5/2024
Like many hospitals across the country, The Valley Hospital in Paramus, N.J., experienced a period of low staffing in its sterile processing department (SPD) combined with high costs associated with agency dependence.
Valley leadership questioned how they could get to the root of the problem and find a solution to reduce agency dependence while hiring full-time employees. “State certification requirements [New Jersey requires certification for SPD technician employment] made staffing the department a major challenge,” says Donna Lagasi, RN, BSN, MS-HCM, CNOR, assistant vice president of interventional services at The Valley Hospital.
To the team’s surprise, the solution was already being implemented throughout the health system: a career development program that aimed to help Valley staff who were looking for guidance, mentorship and sponsorship on their respective career paths. This existing career development program also hosted a career fair highlighting positions that were either in high demand or were available for internal staff to transfer to with minimal or no additional schooling required. Amina Omar, CRST, CHL, Valley’s SPD manager, participated in this career fair, and her presence garnered a lot of interest in SPD roles. That interest led to a key question. “We asked ourselves, ‘Could we create a similar program to train and cultivate our own staff?’” says Ms. Lagasi.
And thus, Valley’s Extern Program was born. “Our team developed a program that provides paid on-the-job training where each extern can achieve their training hours for certification eligibility,” says Ms. Lagasi. “It fostered diversity and inclusion by providing a supportive and inclusive learning environment where all employees, regardless of their background, can thrive and grow.”
Any facility can come up with a great idea for a program, but it was The Valley Hospital’s journey from a simple, can-we-do-it-ourselves question to a successful extern program that advances diversity and solves the SPD’s staffing problem that earned the hospital this year’s OR Excellence Award for Diversity, Equity & Inclusion.

Once the idea was distilled into an actionable plan, Ms. Lagasi and her team sought and ultimately gained approval from upper management before creating the actual training for its externs. “You need to ensure the curriculum includes class time and on-the-job training from established educators,” says Ms. Lagasi. To that end, the hospital was fortunate to have an on-site SPD educator, Dannie Smith, CRST, CID, CER, CHL, BS, as well as a perioperative nurse, Michele Dembin, RN, BSN, who was also a professor at a local trade school, put together a variety of training modules, workshops and additional resources for the class of externs.
The curriculum consists of approximately 60 hours of classroom education — eight of which are scheduled each week — and is taught by the aforementioned SPD educator and OR nurse. The remaining four workdays place the externs in a clinical setting to ensure they receive the 400 hours needed for certification. After passing the SPD certification exam — something that each extern is required to do within one year of enrolling in the program — externs are automatically placed in the role of certified SPD technician and granted an increase in salary. The program also requires all externs to sign a contract agreeing to a two-year minimum commitment from the date of their certification. By any standard, The Valley Hospital’s extern program has been an overwhelming success. In January, the first class of externs graduated from the program, and The Valley Hospital added four fully certified and highly motivated SPD technicians to its sterile processing department, each of whom have acclimated seamlessly with the team.
The second class, which started in March and finished in July, saw six externs graduate from the program — one of whom has already achieved certification (the remaining externs are scheduled to sit for certification in the next few months). Most impressive of all, however, was the program’s impact on staffing. “After many years, the department is fully staffed and has moved away from agency dependence,” says Ms. Lagasi. “Our internal training program has not only exceeded our goals, but it has also helped to cultivate a stronger, more innovative workforce that reflects the richness of our community.” OSM
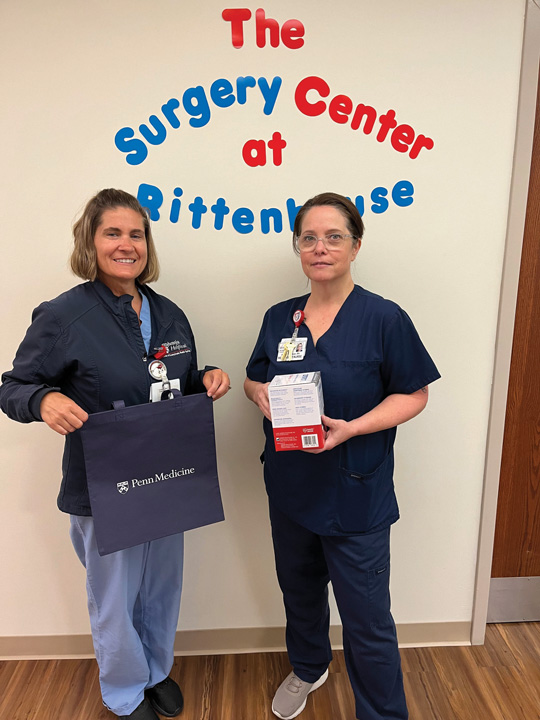
When Susan Walker, DNP, RN, NPD-BC, CNOR, CSSM, CNAMB, and Stefanie Cochran, RN, noticed that several patients frequently seen at The Ambulatory Surgical Center of Pennsylvania Hospital at Penn Medicine in Philadelphia continued to show up to the facility with high blood pressure readings that they were unaware of, they wanted to do something about it. After all, these patients were unmonitored and untreated by their physicians. They were at risk.
“We wanted the patients to be able to track their trends, and we wanted a way to refer them for further evaluation if needed,” says Dr. Walker. The pair put their heads together and searched for a program to partner with, ideally one that could provide what they could not. Ultimately, they decided to team up with Penn Medicine’s medical school research team and to enroll eligible patients in a research study using evidence-based interventions that could improve hypertension rates in a primary care outpatient clinic.
After applying for and being awarded a $2,500 Harrison Fund grant to supply Self-Measured Blood Pressure (SMBP) monitors, Dr. Walker and Ms. Cochran began distributing them to patients with hypertension to make blood pressure monitoring more convenient and accessible for this vulnerable, at-risk population. When prospective patients are enrolled in the study, the Penn ASC team measures process improvements, outcomes and patient experience. It’s a non-randomized study that gives patients the opportunity to try a new, non-medication procedure to reduce their blood pressure. If a patient is deemed eligible at the end of the screening period, their study will last for approximately five years.
“Our initiative targeted at-risk and underserved patient populations through non-typical identification methods,” says Dr. Walker, adding that the project had a greater impact than what was first envisioned.
“The program reached beyond the patient and into extended family members, where multiple people within the same household identified hypertensive patterns using the free blood pressure cuff,” says Dr. Walker. The team at The Ambulatory Surgical Center had the opportunity to get patient feedback in real time from patients returning for duplicate interventions. The study even helped Dr. Walker identify some of her own faulty beliefs regarding hypertension prevention. “I assumed that financial restriction and access were the only barriers to blood pressure monitoring,” she says. “But we were also able to serve patients whose only barrier was ego, those who’d say, ‘I can’t possibly have a blood pressure problem.’”
—Jared Bilski
The holiday season can throw some employees off track, draining their levels of engagement and enthusiasm for their jobs at the end of a long year....
While this year’s celebration of America’s nearly 74,000 Certified Registered Nurse Anesthetists (CRNAs) and residents in nurse anesthesiology programs technically runs...
The Association of periOperative Registered Nurses (AORN) is pleased to announce the appointment of David Wyatt, PhD, RN, NEA-BC, CNOR, FAORN, FAAN, as its new Chief Executive Officer...