- Home
- Article
Going Smoke-Free: What I Wish I Knew
By: Stephanie J. Jones, MSN, RN, CNOR
Published: 10/12/2023
Establishing a clear policy, trialing equipment and opening smoke evacuation supplies for every case has helped us sustain clean OR air.
Achieving smoke-free ORs in the procedural setting at PIH Health Downey (Calif.) Hospital was one of the hardest practice challenges I’ve led — but also one of the most rewarding. Since earning AORN’s Gold Go Clear Award in 2021, we have sustained smoke-free ORs across our entire hospital.
Blueprint for success
With so many states passing smoke evacuation laws across the country, many of my fellow surgical facility leaders are contemplating how to tackle the challenges to make every OR smoke-free. My simple advice to my colleagues is this: Don’t do it alone. Get creative with what you have (and what’s already been done) and remember your reasons for going smoke-free: to create a safe work environment for your team and for your patients. Here is a list of the most valuable tips and tricks our team learned through our smoke-free journey.
• Build the right team. Once we decided to go for AORN’s Go Clear designation, we gathered a team, starting with our existing Surgery Partnership Council, which included the clinical director of surgery (myself), RNs, surgical technologists, the surgery educator and physician representatives from surgery and anesthesia. We then added our materials coordinator to advise on smoke evacuation equipment, supplies and purchasing.
Tip: From the start, be sure to include representatives from interventional radiology, labor and delivery and the cardiac cath lab. To officially earn the Go Clear designation, every area of the facility where surgical smoke is generated must meet all smoke-free requirements, including smoke evacuation and the education of every team member on surgical smoke hazards with competency validation. Having a solid project team really helped during implementation once we identified our challenge areas so we could delegate team members to divide and conquer. These council colleagues have also proven valuable champions, keeping up the smoke-free conversation in their respective circles and daily huddles, which has helped us to sustain 100% compliance with our smoke evacuation practices.
• Do your homework. Understanding and disseminating the evidence on surgical smoke hazards is essential to secure buy-in. We found team members knew smoke was bad for them but didn’t know just how bad. Seeing peer-reviewed research demonstrating the reality of virus transfer, such as HPV released in surgical smoke infecting the respiratory tract of surgeons, was eye-opening.
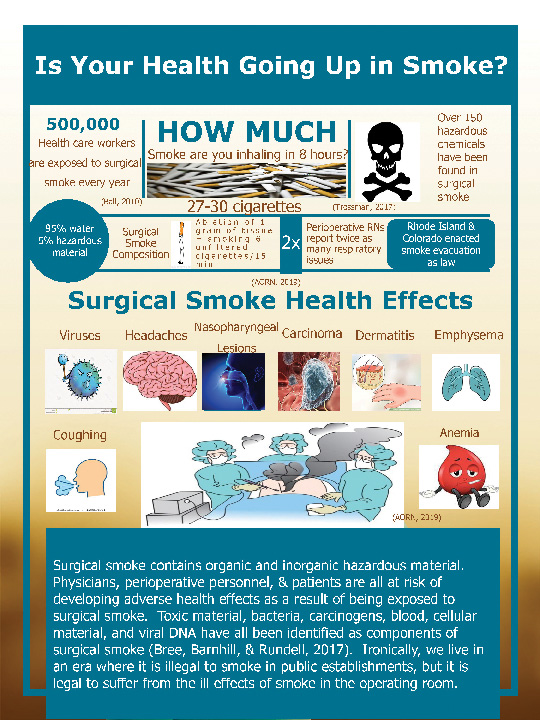
INSTANT IMPACT Visual aids and infographics are effective ways to drive home the many dangers of surgical smoke.
We shared our research in various formats to maximize knowledge and understanding. For example, we shared a one-page visual fact sheet (see graphic, right) during in-service trainings on surgical smoke hazards. It gave people a takeaway with poignant smoke hazard facts.
Tip: We recruited our nurses in BSN and MSN programs to work on smoke hazards as part of their program research because they already had access to the literature. It also proved valuable to recruit a team in the research process to share the evidence on smoke hazards.
• Use equipment you already have (or can easily get). Securing a capital expense approval to purchase smoke evacuation equipment can be challenging. However, most facilities may already have equipment that can be used for smoke evacuation — as was the case for us. We had recently purchased a waste management technology system for every OR suite that included smoke evacuation functionality. We brought the vendor in for additional training, and our materials coordinator took the lead on purchasing additional smoke evacuation supplies. Our OR educator then led the training on how to safely use and dispose of biohazard items such as smoke evacuation tubing and manifolds.
Tip: If you apply for capital purchase approval and are denied, try submitting smoke evacuation as a safety project for funding through your organization’s foundation. Sharing the facts on smoke evacuation for a safe work environment can help to encourage foundation funding.
• Trial smoke evacuation equipment to find the right fit(s). The most common concerns we heard from surgeons about using smoke evacuators was that the evacuation pencil was bulky and challenging to use, and the noise of the system was distracting. To address these concerns, we connected with vendors to bring in different smoke evacuator pencils and gave surgeons the chance to test and vote for their favorites. We purchased their two favorite pencils. This helped secure surgeon buy-in by engaging them in the process and respecting their preferences.
• Be strategic about gaining champions. Once we had introduced our plan to the entire perioperative team and had smoke evacuation equipment ready to use, we started targeting education to specific teams for buy-in. We wanted our RNs and surgical technicians comfortable with how to open, use and discard smoke evacuation disposables. We also wanted them to be the experts in the room to troubleshoot device use. Then we went to each individual group committee meeting, including anesthesiologists and surgeons to explain our project, its timeline and address any concerns.
Tip: We had tremendous success with securing buy-in with our anesthesiologists. They are a smaller group of physicians who are in the room for multiple cases every day, exposing themselves to surgical smoke for extended periods. They became invaluable champions for the smoke-free cause.
• Establish your smoke-free policy early on. Having a specific policy dedicated to the detailed practices of smoke evacuation does two important things. First, it standardizes the “how” to help teams get it right every time, such as how closely to hold the device to the body to prevent smoke from escaping into the room. Second, a policy is something everybody can reference to empower practice, a document that makes it clear compliance isn’t optional.
Tip: To help achieve compliance, we encouraged the scrub tech to open smoke evacuation devices for every case, regardless of surgeon preference. Although this seemed a bit of a gamble, the surgeon was far more likely to use the already-open smoke evacuation devices to avoid needing to discard them and waste supplies. After we started opening smoke evacuation supplies 100% of the time, compliance rose considerably.
• Make it a competition. Auditing compliance was an essential piece of helping make smoke evacuation a habit. In the final push of implementation, our auditing identified individual surgeons who weren’t evacuating smoke consistently, so we posted compliance rates in our community lounge for all to see. No one wanted to be at the bottom of the leaderboard. Our weekly compliance updates soon leveled out with everyone at the top, which was a triumph for everyone to see.
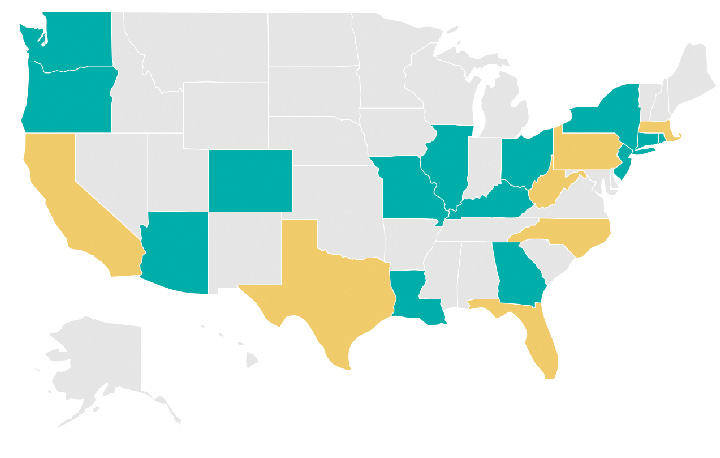
This summer Louisiana, Ohio and Missouri became the latest states to sign smoke evacuation bills into law, joining Arizona, Colorado, Connecticut, Georgia, Illinois, Kentucky, New Jersey, New York, Oregon, Rhode Island and Washington. “With most of these laws passing in the last two years, we see the momentum for requiring smoke-free ORs ramping up significantly,” says Jennifer Pennock, associate director of AORN Government Affairs.
“While the wording and specific requirements for surgical smoke evacuation laws vary between states, one common thread is the focus on the health and safety of the OR staff, especially after all we’ve learned about respiratory health in the past few years,” says Ms. Pennock. “When a nurse works in a state with a smoke evacuation law on the books, this means they are protected from the hazards surgical smoke presents during surgery, which is a win for nurses, other members of the surgical team and even patients.” Ms. Pennock is working closely with nurses across the country to prepare for introducing smoke evacuation legislation in the 2024 state legislative sessions.
Track the current status of enacted and pending smoke evacuation laws in your state with AORN’s National Map of Current Surgical Smoke Evacuation Laws and Legislation at osmag.net/map.
—Carina Stanton
• Sustain compliance. An important part of earning the Go Clear award is sustaining smoke evacuation compliance through ongoing competency training and auditing. We also have our award posted prominently in our main OR hallway to help new and established team members keep smoke-free practices in mind, and it is something everyone has come to expect and champion.
Recently, a colleague from the cath lab knocked on my door to ask me why there was a smoke smell in the air. I investigated and suggested the team hold the evacuation device closer to the surgical site. This moment solidified for me that we truly work in a smoke-free culture with zero tolerance for any surgical smoke exposure, which is a very exciting place to be.
Did you know that many of the resources needed to go smoke-free have already been created? Here’s a short list of resources available at aorn.org for every step of the journey:
- Go Clear Award & Center of Excellence in Surgical Safety: Smoke Evacuation Program with complimentary team education and compliance monitoring tools. Learn more at osmag.net/clear.
- Management of Surgical Smoke Tool Kit with team education and informational posters on the evidence of smoke hazards.
- Policy template to make smoke evacuation a required practice.
- Gap analysis to understand smoke evacuation-specific areas for improvement.
- Competency verification tool to improve knowledge and confidence with smoke evacuation practices.
- Evidence table with research citations from AORN’s Guideline for Surgical Smoke Safety.
—Carina Stanton
• Sell smoke-free to recruit and retain staff. We are very proud to be smoke-free and discuss it with every perioperative candidate we interview. Being smoke-free has become a benefit of employment here, which also makes it a powerful recruitment tool — once you experience working in a smoke-free procedural setting, it would be difficult to work in a smoky environment.
I am proud that we provide a healthy work environment with clean air, instead of OR rooms filled with smoke. We are no longer plagued by eye and nose irritation, headaches and scratchy throats — we have truly cleared the air and removed surgical smoke for good. OSM
.svg?sfvrsn=be606e78_3)
.svg?sfvrsn=56b2f850_5)