Nine Ways to Make an Outpatient Hip Program Flex
By: Adam Taylor | Managing Editor
Published: 3/3/2025
It’s often the components surrounding the procedure — not the surgery itself — that bring value-added elements that lead to success.
While there are many important considerations for running a top-notch outpatient total hips program, what happens in the OR is fairly straightforward and not necessarily on the top of the list.
Holistic approach
“I think people tend to concentrate only what happens in the ASC’s operating room, which is probably less important than focusing on the other phases of care,” says Mathias Bostrom, MD, associate surgeon-in-chief and director of quality and safety at Hospital for Special Surgery (HSS) in New York City. “Concentrating on the whole episode of care is what makes for a successful program.”
Doing so will go a long way toward relieving patients’ pain, increasing their mobility and improving their quality of life. Here’s a short list of essentials that ASC leadership thinking of adding a total hip service line should consider.
1. Be conservative with patient selection
The hip surgeons at HSS perform same-day replacements only for the most medically appropriate patients — those with no significant issues with their major organs, healthy BMIs and without anything complicated with the hip itself from an orthopedic standpoint, says Dr. Bostrom.
“Our bias is to land on the conservative side,” he says. “Including patients who don’t meet stringent medical screening isn’t going to work out.”
Steven Schultz, MD, of the Oklahoma Center for Joint Replacement Surgery in Norman, also sticks to younger, more active and healthier patients who won’t need an inpatient rehab after they get their new hips.
“Clearly, you can’t do an outpatient hip with a patient on dialysis or a 90-year-old lady with heart issues,” he says. “I’m very conservative with my patient pool, in part because of our location, where patients don’t necessarily have an expectation of going home. If I were in New York City, Dallas or LA, I might have to expand it, but there’s no need to talk a 75-year-old farmer into going home if he feels more comfortable staying overnight. Even though I could be more lenient, if you go too far you could just end up with people coming back with complications.”
2. Include the patient’s support network in pre-op education

Knowing what to expect — and managing those expectations — goes beyond the patient.
“You need the buy-in of the patient and the patient’s support network, whether it’s a spouse, child, friend or someone they’ve hired to help them after the surgery,” explains Dr. Bostrom. “I’ve had patients who plan to go home that day, and it was a surprise to the loved ones. They could be unprepared or apprehensive about it, the latter of which is reasonable, as a 250-pound patient might be too much for a 130-pound loved one to responsibly care for in the days after surgery.”
Dr. Schultz also includes the patient’s support network in pre-op visits. “Certainly, an educated patient and loved one who know what to expect makes recovery much easier,” he says. “About 75% of our patients have someone who will help to take care of them, so we need to make sure they’re willing to do so and comfortable with it. For the 25% who go home to a house where they live alone, their preoperative education is even more critical.”
3. Specialists do it better
The advice for leaders looking for surgeons to practice at their facility is the same as what’s given to patients looking for doctors: Find the ones who do nothing else but hip and knee surgeries. “Like anything else in life, practice makes perfect,” says Dr. Bostrom.
“You’re going to have better outcomes if you’re at a facility that does a lot of total joints,” adds Dr. Schultz. “The outcomes will be better at a place that does 1,000 a year versus a place that does two a month. And the complication rates will be lower if you have a surgeon who does several hundred a year versus one who does one or two a month.”
4. Use regional anesthesia
It’s possible to perform total hips without using nerve blocks, but not ideal.
“Having an anesthesia team proficient in regional anesthesia is a critical aspect of the operation,” emphasizes Dr. Bostrom. “We think regional blocks are superior in terms of immediate postoperative pain relief and get people up much easier than if we used just general anesthesia. It slows down the process a little bit, but I think it’s safer in general and overall patient satisfaction is much greater.”
Specialized pain management for anesthesiologists at HSS means using very focused local nerve blocks in addition to the larger regional blocks, as well as a postoperative cocktail.
Dr. Schultz also employs regional anesthesia in combination with spinal or general anesthesia, depending on the surgery center he’s at on a given day. He also performs injections of a pain cocktail deeply and superficially in the site around the hip for additional postoperative pain control.
5. Plan with the end in mind
Physical therapists visit all HSS patients preoperatively to explain what their aftercare regimen will include, says Dr. Bostrom. Including this in the pre-op assessment/testing process is important, as how patients work to recover plays a key role in their ultimate success. Patients are contacted regularly in the first day or two after the surgery to make sure they’re doing well and following their discharge and rehab instructions.
“The appropriate postoperative follow-up from the surgery center or the surgeon is essential to making sure that nothing is wrong in the first day or two after the surgery and that the wheels are still on the tracks,” says Dr. Bostrom.
A physical therapist or nurse will take Dr. Schultz’s patients through a series of exercises two or three hours after surgery. How well they do helps determine when they can go home. Patients will continue their physical therapy at an outpatient location or have a provider come to their home.
6. Standardize procedures and maintain team continuity

Dr. Bostrom suggests not having multiple operating systems in the OR. Having one or two ways of doing things and making sure everyone understands them is the preferable option.
“In terms of the OR team make-up, you need a circulator, a first assist and preferably a second assist as well — and they have to work as a team,” he says. “A good team that’s been together for a while makes your day go very smoothly. You can tolerate one new person on the team, but if it’s more than that or if there’s a team you’ve never worked with, that could make for a long day in the OR.”
The industry rep should make sure you’re not waiting for an implant and other facility personnel must ensure that the room is set up properly and on time, says Dr. Bostrom. “The industry rep provides an important service, even though they’re not employed by the facility or the surgeon’s medical practice,” he says. “They make sure the implant and other inventory is there, and if there’s any degree of technology such as computer navigation or robotics being used, they’re responsible for it being in working order.”
7. Specialized training
OR and PACU nurses need training specific to total joint procedures, says Dr. Schultz.
“The OR nurses need to know how to safely transfer the patient from the operating table to the other bed,” he says. “Patients can have their new hip dislocated during this process if their legs are twisted because they aren’t kept straight.”
There are also different ways to handle a patient depending on whether their surgery was performed with an anterior or posterior approach, he says. PACU nurses need to be trained in the different methods, particularly if they’ve never worked with joint-replacement patients before.
“One of the surgery centers I work at is about to start a joint program, so we’ve had a couple physical therapists come over and meet with the PACU nurses who are used to doing shoulder scopes, knee scopes, ACLs and other common outpatient cases, but who have never seen a total hip performed unless they worked at a hospital previously,” says Dr. Schultz. “They need to know how to handle these patients when they’re out of the acute phase of recovery and into the next phase when they’re getting up to walk or go to the bathroom.”
8. Integrated ORs, robots and special tables aren’t required
- Mathias Bostrom, MD
Guard against outfitting new service lines with the latest top-of-the-line gadgets that have all the bells and whistles.
“I think physicians who are starting a new hips program need to know that, while we all use varying degrees of technology, there’s a cost to all of it and some of it is quite expensive,” notes Dr. Bostrom. “If you’re running an ASC, cost is important, because as an owner you want to minimize costs. These technologies add costs and maybe do not include an increased benefit.”
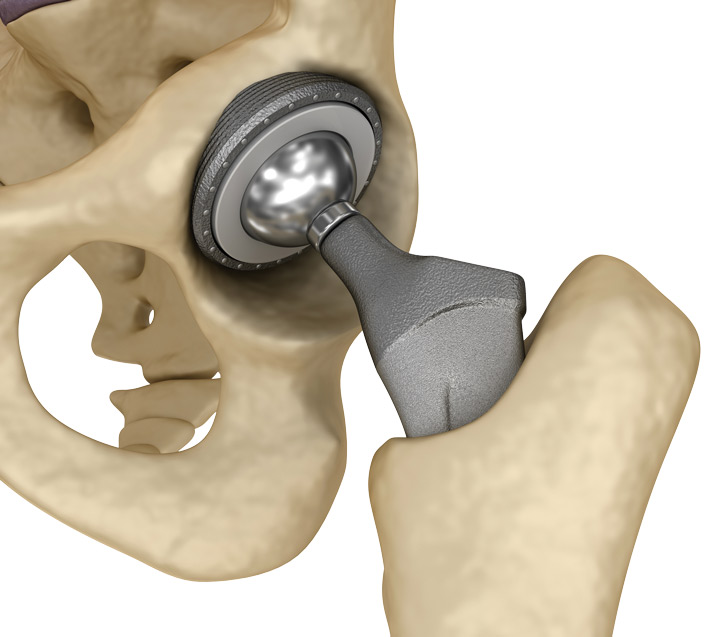
Dr. Bostrom does, however, use computer navigation systems fairly regularly to position the cup of the implant. Dr. Schultz sometimes uses computer navigation if the ASC he’s working at has such a system, but he isn’t dependent on it. The same goes for robots. He recently used a robot for a total hip case because the patient’s femur was shaped irregularly from childhood deformities. The robot helped ensure he achieved the correct alignment for the hip implant.
Choosing surgeons who are flexible is also important, say the doctors. Some can’t perform total hips without a robot or a specialized table.
9. Fine-tune pre-, intra- and postoperative functions
Focus on the pre-op and post-op components of cases and keep the surgeries themselves comparatively uncomplicated, says Dr. Bostrom.
“You want to do the cases we call ‘chip-shot hips,’ meaning comparatively simple cases,” he explains. “You won’t have the equipment at most ASCs to revise things intraoperatively if there’s a problem, so the procedures should be straightforward from a technical standpoint.”
Again, this is why patient selection is so important. Complex primary hips aren’t appropriate for ASCs, and severe complications can be avoided by not working on the wrong patients at those facilities. Proper patient selection is the key.
“The actual implants, for example, don’t have a major impact on outcomes. A hip is a hip,” says Dr. Bostrom. “If I have a patient with poor bone quality that’s so bad that I need to cement a hip, that person isn’t a candidate for an outpatient procedure at an ASC.”
Multiple benefits
A good outpatient program not only makes for happier patients, it’s also good for business, notes Dr. Schultz.
“Surgery centers tend to be more efficient than hospitals and that’s whether the procedure is inpatient or in an HOPD,” he says. “I don’t know if it’s the employees or the demands of the employer, but I can do five or six totals at Dr. Keith Smith’s Surgery Center of Oklahoma and be out of there in five or six hours. If I do those five or six cases at the hospital, I’ll be there 10 hours.” OSM
.svg?sfvrsn=be606e78_3)
.svg?sfvrsn=56b2f850_5)