Pay Attention to Trends
Leaders juggle so many different tasks and responsibilities every day, including their own professional development....
This website uses cookies. to enhance your browsing experience, serve personalized ads or content, and analyze our traffic. By clicking “Accept & Close”, you consent to our use of cookies. Read our Privacy Policy to learn more.
By: Kristin Truesdell
Published: 4/2/2024
For 15 years, cardiovascular procedures have been performed in outpatient settings such as office-based labs (OBLs) and ASCs, starting with peripheral vascular (PV) and device implant procedures. Reflecting clinical advances, CMS added coronary procedures to its ASC Covered Procedure List (CPL) in 2019 and 2020, which allows reimbursement for diagnostic cardiac catheterizations and low-risk percutaneous coronary intervention (PCI) in ASC settings.
Recently, the flow of additional cardiovascular procedures to ASCs has slowed. That’s due to several factors. The COVID-19 pandemic began the same year PCI was added to the ASC CPL. Cardiovascular services remain highly regulated in many states. Hospitals remain hesitant to shift volume from HOPDs to ASCs due to decreased reimbursement.
Despite those barriers, my consulting firm, Corazon, has seen same-day cardiac adoption grow with an increasing number of ASCs billing for PCI procedures. In 2019, only about 30 centers billed for PCI procedures. In 2023, the number increased to approximately 65. There is also burgeoning interest among hospitals, physicians and private investors to investigate how vascular procedures traditionally performed in OBLs and cardiac procedures in ASCs can utilize the same physical space while still reaping the financial benefits of each place of service. This phenomenon has led to the inception of the hybrid OBL/ASC model.
When evaluating which setting of care — OBL, ASC or hybrid — works best for your key stakeholders with this growing outpatient specialty, consider the reimbursement landscape, especially regarding new ASC-only C codes that impact cardiac and vascular procedures.
Using these C codes to identify products, devices and services in conjunction with existing cardiovascular CPT codes expands the cardiovascular work that can be done in ASCs and goes a long way to ensure your billing to CMS is accurate and your reimbursements are complete.
According to the CMS final rule, certain cardiovascular procedures on the CPL have received larger increases in payments compared to the market basket update of 3.1%.
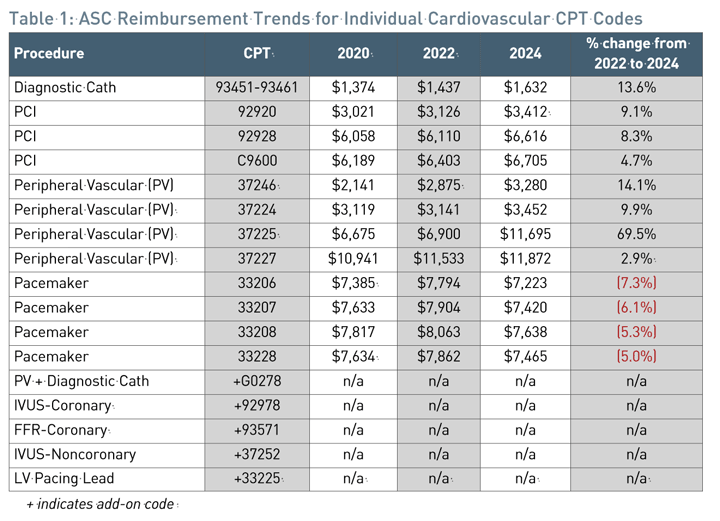
Table 1 highlights reimbursement trends from CY2020 to CY2024 for common cath lab procedures performed in ASC settings. While pacemaker reimbursements declined, diagnostic cath and PCI procedures realized significant increases in payment ranging from 5% to 13% in that timeframe. Note that secondary procedures such as intravascular ultrasound (IVUS) or fractional flow reserve (FFR), when performed in conjunction with a primary procedure such as a diagnostic cath or PCI, must be coded even though such add-on codes have a payment indicator of N1, which means it is a packaged service/item and no separate payment is made.
Fortunately, CMS adopted a complexity adjustment factor in its CY2023 ASC final rule that increases reimbursement when an add-on code is performed with a primary procedure in certain coding circumstances. CMS C codes are temporary HCPCS Level II codes created for Medicare purposes that revolve around new technology devices, drugs, biologicals and radiopharmaceuticals that have received transitional pass-through status under the Medicare Hospital Outpatient Prospective Payment System. Currently, more than 50 C codes are exclusive to ASC-specific cardiology and PV procedures.
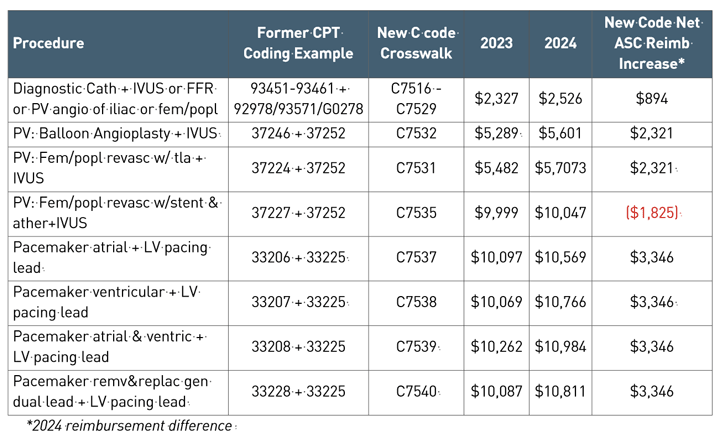
Table 2 shows specific CPT code combinations that crosswalk to the new C codes and shows a comparison of the 2023 and 2024 reimbursement rates. It also highlights the net reimbursement gain, which is designed to offset the cost associated with the add-on procedure.
• Diagnostic cath. With the new C code range of C7516-C7529, an additional $900 of reimbursement can be gained for these cases. Several clinical studies have varying rates of calculated utilization but all hover around 15% IVUS utilization. This does not include the percentage of FFR utilization that would enhance the overall number of patients eligible for the new C code assignment.
• Peripheral vascular. The use of IVUS in peripheral interventions has grown significantly in recent years. In fact, IVUS utilization for PV procedures was greatest in ASCs and OBLs, with 40% utilization according to one recent journal article. For C7531 and C7532, an additional $2,321 of reimbursement can be gained for these specific cases. Oddly, net reimbursement declines of $1,825 occur for C7535. This code is level 4, which is the ceiling for pricing so it will max out. Theoretically, if a significant volume of claims are submitted for this code, it should drive up the Level 4 APC reimbursement rate for the next year.
• Pacemaker. Despite reimbursement declines of the traditional pacemaker codes (33206-33208), the new C codes provide an additional $3,346 in payment, which is the most significant net increase of all cardiac and vascular C codes. The pacemaker C codes now even reimburse a few hundred dollars higher in the ASC setting than in the HOPD setting.

Compared to specialties such as GI, ENT and general surgery, performing cardiac and vascular procedures in an ASC is relatively new. Coding for these procedures requires expert resources and the adoption of the new C codes, which add a layer of complexity for the coding team. To help ensure your team codes and bills the new C codes properly, remember:
• The new C codes are only allowable and payable in an ASC.
• When a primary procedure and secondary add-on procedure code occur during the same encounter, the new C code must be billed rather than the individual procedure codes. Keep in mind that C codes are only applicable for a particular set of coding combinations.
• In certain scenarios, a combination of C codes and Category 1 Codes will be necessary, especially when reported with PCI codes. Verify that the modifier is appropriate when performing a diagnostic cath and PCI in the same encounter.
• Inform the ASC director, clinical staff, coding teams and physicians of the changes and provide ongoing education about them.
• Update all templates and documents such as pre-auth checklists, chargemaster, physician operative note templates, fee schedules and any pre-build report within the EHR.
• Audit charts to ensure proper documentation, code assignment and reimbursement.
—Kristin Truesdell
While standalone OBLs and hybrid OBL/ASC models have gained traction and success, the question is long-term sustainability. As CMS continues to add more procedures to the CPL, increase ASC reimbursement and add new bundled C codes specific to ASC settings, the evidence favors an ASC-only model in the future. This trend will likely speed the conversion of hospitals from OBL or hybrid to ASC, even among organizations that have traditionally resisted the shift from HOPD to ASC. The newly adopted C codes can also spur volume growth at current ASCs that offer cardiac and vascular procedures.
As long as ASC reimbursement rates remain favorable, I believe there will be a significant impact on strategic decision-making for outpatient surgery leaders.
The current reimbursement environment not only highlights the financial implications but also emphasizes the importance of strategic planning to manage the complexities of cardiac procedures within ASCs. By proactively incorporating cardiology codes into their operational framework, ASC leaders can position their facilities for long-term success, ensuring that patients receive optimal care while maximizing financial viability in this ever-changing healthcare landscape. OSM
Leaders juggle so many different tasks and responsibilities every day, including their own professional development....
For an easier day in the OR for small bone cases, CONMED has developed a new system that delivers improvements without drawback and convenience without trade-offs....
“Say goodbye to endless waits in the emergency room — New Yorkers now have a fast solution for their urgent orthopedic needs at our Orthopedic Urgent & Sports Medicine...