- Home
- The Magazine
- Article
A Nose for Reducing SSIs
By: Danielle Bouchat-Friedman | Senior Editor
Published: 10/5/2023
Why universal nasal decolonization should serve as a staple of every facility’s infection prevention bundle.
Finding an easy-to-implement, cost-effective and widely accepted patient-approved infection prevention protocol to help prevent surgical site infections (SSIs) is no small feat.
Despite being backed by strong evidence, nasal decolonization is less understood and practiced than preoperative skin bathing with chlorhexidine gluconate (CHG). That’s surprising, considering clinical evidence demonstrates that 80% of S. aureus that can cause SSIs is found inside a patient’s nose. Here’s how to create a nasal decolonization protocol to ensure team buy-in and patient compliance.
Addressing the issue
Kimberly Candray, CIC, BS, MT (ASCP), infection prevention manager at Northwest Medical Center, a 300-bed, for-profit hospital in Tucson, Ariz., that performs 30 to 50 surgeries a day, keeps a close eye on her patients’ SSI rates. When she noticed SSI rates were .58/100 for spine fusion patients and .46/100 for laminectomy patients, higher than expected, she decided to dig a little deeper to determine the cause. As it turned out, even though nasal decolonization with povidone-iodine (PVI) was part of the infection prevention bundle, patients weren’t complying. “Patients did not like the PVI method,” says Ms. Candray. “They complained that it burned their noses, so they would often refuse to use it prior to their procedure.” The yellowish stain that it would leave underneath their nose was also a deterrent.
In response, Ms. Candray decided to switch to an alcohol-based nasal antiseptic for three months to see if spine patient compliance improved and, in the process, lower the rate of SSIs. Decolonization was part of an already robust infection prevention protocol that included CHG bathing at home and in pre-op. “We were already advising all our patients to take baths with CHG before they came in for surgery,” says Ms. Candray. “Then once they got into the preoperative area, we would wipe them down again with CHG foam.” Then, an alcohol-based nasal antiseptic was applied to the nares of all spine surgery fusion and laminectomy patients within one hour of surgery, instead of the PVI nasal antiseptic that had been in use previously.
She says patients’ positive reactions to the alcohol-based nasal antiseptic were almost immediate. “I had patients tell us they felt like they had a little spa in their nose,” says Ms. Candray. After three months, she checked to see if the change had any effect on SSI rates. “I really didn’t have any preconceived notions about what the results might be after making the switch. I was hoping patients would respond to it and in turn, comply with nasal decolonization prior to their procedure, but I was pleasantly surprised when I noticed our rate of SSIs decreased.” Indeed, SSI rates for spine fusion decreased 64%, from .58/100 to .21/100 patients. For laminectomy procedures, there was a whopping 100% reduction in SSIs.
After making the switch from PVI to the alcohol-based nasal antiseptic, the facility also enjoyed another benefit: saving money. “In one year, we were able to save $37,000 alone, just by switching to a less expensive product. We also estimated that the switch saved us another $127,000 by avoiding a potential infection associated with nasal decolonization non-compliance,” says Ms. Candray.
Standardization improves compliance

Nursing Business Strategist Carrie E. White, MSN, RN, CAPA, was concerned about two hospitals in Central Virginia that struggled with an elevated SSI rate related to colorectal surgeries and decided to take a closer look. Even though the hospitals were using antibiotics and CHG wipes, nine colorectal SSIs still occurred in 2020.
In response to the SSIs, leadership formed an interdisciplinary committee with representation from nursing leadership, infection control, a general surgeon and process engineering support, with the goal of developing a plan to decrease the SSI rate for colorectal surgeries.
A literature review was completed to assess what type of colorectal bundle could be started to reduce infections. “The review suggested the following interventions for consideration: the use of antibiotics, chlorhexidine wipes or baths, separate closing clean instrument tray, normothermia with forced-air warming, nasal decolonization with PVI swabs and bowel preparation,” says Ms. White.
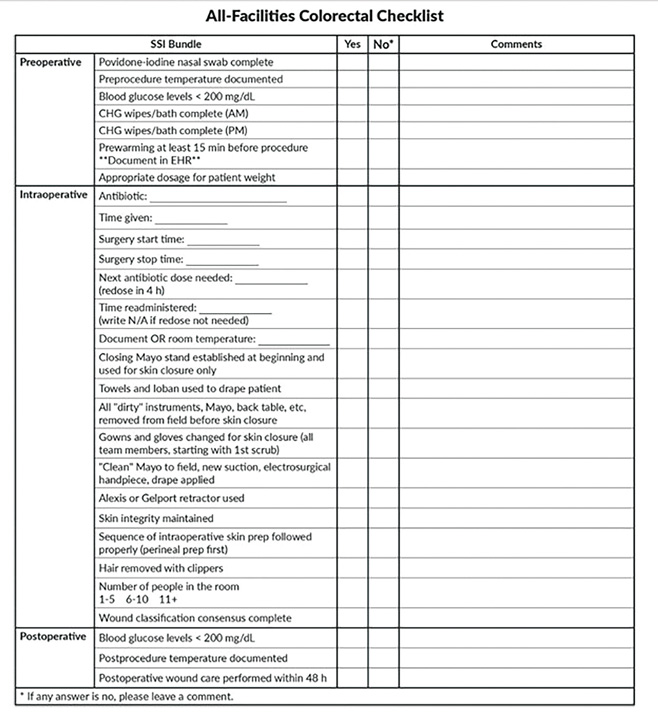
After the bundle was developed, the interdisciplinary team also developed a handy checklist that guided staff on the standard practice of the SSI prevention bundle. The checklist spells out which part of the SSI bundle needs to be implemented preoperatively, intraoperatively and postoperatively. For example, patients must swab their nose with PVI preoperatively.
The checklist was implemented in January 2021, and Ms. White says it helped provide a standardized SSI prevention process for staff. “After implementing the bundle, we had positive effects and improved our SSI rate from an annual total of nine down to just three over a 12-month period,” she says.
To successfully implement an infection prevention bundle, Ms. White says it is necessary to get key stakeholders to participate in the initiative. “Staff and surgeon engagement in all areas of surgical services was a necessity for successfully implementing a colorectal bundle,” she says, adding that auditing the process and remaining open to feedback and suggestions were other key factors in the success of the initiative.
Change that sticks
If universal nasal decolonization isn’t feasible at your facility, Ms. Candray says it’s OK to focus your efforts on high-risk procedures, such as implantable devices, cardiac procedures and spine surgery. “We decolonize any patient who gets an incision because the body has bacteria all over it,” she says. “But 80% of the bacteria that’s on the body is actually breathed out through your nose, so why would you decolonize the body and not decolonize the nose as well?”
While getting buy-in from staff on the importance of implementing a universal nasal decolonization program at your facility is important, it’s only one part of the equation. You also need to educate patients on why it’s so important, says Ms. Candray. Make sure your team understands the evidence-based rationale behind nasal decolonization to ensure it occurs consistently and to help staff answer questions about something that can seem a bit strange to patients who are naïve to the concept. “Patients often don’t understand why facilities ask them to decolonize their nares before their procedure,” says Ms. Candray. “They don’t realize just how important it is to prevent SSIs and send people home happy and healthy.” And yes, the cost savings associated with decolonization are nice, too. Saving a few bucks is always good for the bottom line, but achieving greater patient satisfaction for something that takes just seconds to do it is worth its weight in gold. OSM
.svg?sfvrsn=be606e78_3)
.svg?sfvrsn=56b2f850_5)