Communication Is Key for All Situations
As the leader, you may need to communicate bad news to your team as changes or situations occur....
This website uses cookies. to enhance your browsing experience, serve personalized ads or content, and analyze our traffic. By clicking “Accept & Close”, you consent to our use of cookies. Read our Privacy Policy to learn more.
By: Joe Paone | Senior Editor
Published: 9/25/2024
In May, Minnesota became the 18th U.S. state to pass a surgical smoke evacuation mandate into law. In June, a hospital in neighboring North Dakota, a state where such a bill has not passed or even been introduced, took inspiration from the legislative action next door and mandated to its own providers that evacuation systems must be used for every smoke-producing procedure in its ORs.
Jamestown (N.D.) Regional Medical Center (JRMC) says it is the first facility in the Peace Garden State to implement such a policy, which actually puts it ahead of the Minnesota law that goes into effect Jan. 1, 2025.
“While the research on the risks of surgical smoke is still evolving, we want to do everything in our power to safeguard those in our care,” stated JRMC President and CEO Mike Delfs, MBA, when the policy was announced to the public. “Going smoke-free aligns with our dedication to leading with science and pursuing the highest standards of clinical excellence.”
By publicly announcing its policy, JRMC reiterated to its patient population that it is laser-focused on safety, while smartly signaling to perioperative professionals in its area that they don’t need to stay in Minnesota to work in smoke-free ORs. Perhaps most importantly, of course, it was a huge breath of fresh air for its own perioperative staff, who had become increasingly concerned about the impact of surgical smoke exposure and had been building the case for an evacuation policy.
“June 1 was our official ‘smoke-free day,’ but we had been working on it for several months,” says Rhea Miller, RN, JRMC’s surgical services manager.
In recent years, the potential harm of surgical smoke was informally discussed among JRMC surgical staff. “Every once in a while, depending on the procedure, we could smell the cautery smoke out in the hallway,” recalls Ms. Miller. “We kind of just had it in the back of our heads that it probably isn’t the best thing.”
Several years ago, a JRMC general surgeon who had worked in ORs for 35 years was diagnosed with throat cancer. Staff wondered about the role of surgical smoke exposure in the physician’s condition. “The thought was that the surgical smoke was one of the contributing factors to his throat cancer, because he never smoked or anything like that,” says Ms. Miller.
While the potential role of surgical smoke in the surgeon’s case was never confirmed, the unfortunate diagnosis served as a catalyst that eventually led to the hospital’s institution of its smoke evacuation policy. “Once we started talking about it, I think that got more people thinking about it too,” says Ms. Miller.

Like many facilities interested in going smoke-free, much of the equipment JRMC needed to evacuate the toxic plume was actually already in-house. JRMC’s transition required minimal financial investment, as once its existing suction and ventilation system was equipped with the appropriate attachments, all its OR teams needed to do was turn the system on before every smoke-producing case to safely evacuate surgical plume from its ORs.
In fact, some of JRMC’s surgeons and their teams had already been employing smoke evacuation during cases. “Certain procedures would produce more smoke than others, and certain surgeons used it more than others,” says Ms. Miller. “We were using smoke evacuation on probably half of our smoke-producing cases at that time.
“Our OR suction machines already have ULPA [ultra-low particulate air] filters, which filter all of the bad stuff in the air, built right into them, and we already had the correct tubing to use for that,” says Ms. Miller. “We just needed some new blades that would attach to the correct tubing. And honestly, that was all we really did. We just had to get some different end attachments for that tubing.”
What turned this informal strategy into a more comprehensive formal policy was a visit from a rep of one of the hospital’s existing vendors. “She came to our hospital last September and gave us nurses a presentation on the dangers of OR smoke,” says Ms. Miller. “She gave us all the stats about which states have already done this, and all of the states that are in the process of working on it. She really got us thinking, and the more we got thinking about it, we just decided, ‘You know what? We’d just need to change a couple things and we can be smoke-free.’”
That really got the ball rolling, but there was still work to do.
A common refrain of smoke evacuation advocates at both inpatient and outpatient facilities is that many surgeons disallow the use of smoke evacuation systems because they don’t like the tactile feel of the evacuation pencils or the noise that the evacuation system produces. Ms. Miller says that wasn’t an issue at JRMC, especially after physicians got a clearer picture of the damage that surgical smoke could do.
“Earlier this year, I had our vendor rep come back to give the same presentation she gave to us nurses to our anesthesia providers and our surgeons,” she says. “After that, I asked the surgeons, ‘Do you guys all think this is something you can do?’ And they all said, ‘Absolutely.’ We really didn’t get any pushback. I think the presentation kind of changed their minds when they realized the dangers of the surgical smoke.”
The surgeons subsequently tested smoke evacuation options to better determine which equipment worked best for them. “We just had to try out a few different things, and our rep was excellent with helping us through all that,” says Ms. Miller. With the surgeons and anesthesiologists in her corner, the hospital’s C-suite approved the new policy.
This was a simple change that will have a lasting positive impact on our staff.
Robert McMillan, MD
“The use of smoke evacuation cautery was an easy change to make,” says JRMC orthopedic surgeon Michael Dean, MD. “It is much better for safety of staff and has no downside compared to regular cautery.” Adds JRMC general surgeon Robert McMillan, MD, “This was a simple change that will have a lasting positive impact on our staff. It is a testament to the OR leadership that we were able to implement smoke-free operating rooms without any disruption to our day-to-day business.”
JRMC’s OR teams, of course, are pleased about going completely smoke-free. “I think they realize this was definitely a good, healthy move for us,” says Ms. Miller. “I heard a couple of them say, ‘I don’t know if I have as many headaches as I used to at the end of the day,’ and others say they’re not as tired. I definitely think there was a lot of health-related stuff — nothing major, nobody was going home early, nobody was truly sick — just things like they didn’t have a runny nose during the day when they were in some of those heavier cautery-use rooms.”
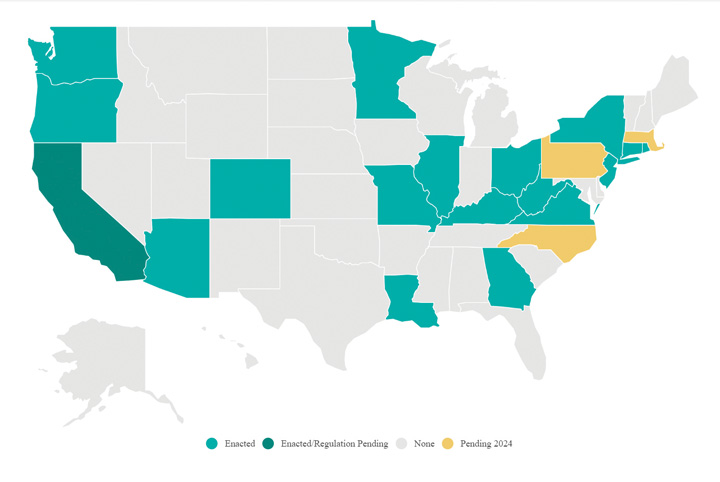
This year, three states — West Virginia, Virginia and Minnesota — became the 16th, 17th and 18th states, respectively, since 2019 to pass surgical smoke evacuation mandate laws.
West Virginia. On Mar. 22, the Mountain State’s Republican governor, Jim Justice, signed HB 4376 into law. The Association of periOperative Registered Nurses (AORN), which has worked tirelessly with its members and other organizations in all 50 states to help advance smoke evacuation legislation, reports the new law will require West Virginia’s Office of the Inspector General to propose rules for legislative approval that will require a healthcare facility to utilize a smoke evacuation system during any procedure likely to generate surgical smoke. Any health facility subsequently in violation will be subject to a fine of $1,000 to $5,000 per violation. The law goes into effect on Jan. 1, 2025.
Virginia. After the commonwealth’s House and Senate passed identical bills — HB 763 and SB 537, respectively — both were signed into law by Republican Gov. Glenn Youngkin on Mar. 28. Virginia’s law goes into effect on July 1, 2025.
The development of the law was a grassroots effort. Janet Shortt, MHSA, BS, RN, CNOR, president of AORN Chapter 4702 in Richmond, engaged the Virginia Nurses Association about the importance of surgical smoke evacuation. The organization agreed and added surgical smoke evacuation legislation to its 2024 policy agenda.
Ms. Shortt offered a public comment on HB 763. “After 20 years in the OR, after three bouts of bronchitis and multiple upper respiratory infections, I was diagnosed with asthma,” she said. “I thought this odd as I was living a healthy lifestyle, working out five days a week and eating a healthy diet. I now have chronic asthma that requires inhalers.” She said surgical smoke aggravates her asthma and makes her eyes water.
In fall 2023, an AORN survey of its Virginia members revealed that 94% of respondents said their facility had smoke evacuation equipment, but only 26% said that surgical smoke was always evacuated during smoke-generating procedures. These results helped drive home to legislators the necessity of a mandate to ensure that surgical smoke evacuation systems are not just present but actually used for every smoke-generating surgery in the state.
Minnesota. On May 17, Minnesota’s Democratic governor and current nominee for U.S. vice president Tim Walz signed omnibus labor and industry policy bill SF 3852 into law. A Jan. 1, 2025, smoke evacuation mandate is part of the new law. The successful passing of the smoke evacuation mandate resulted from a combination of lobbying by groups like AORN and grassroots advocacy from workers in the field, including powerful testimony delivered to the Minnesota House of Representatives’ Labor and Industry Finance and Policy Committee in February by John Zender, RN, a retired firefighter and current perioperative circulating nurse from Crosby, Minn., who works at University of Minnesota Medical Center in Minneapolis.
As always, AORN is offering resources to nurses in these three states on how to ready their facilities for compliance, including the next steps that imminently impacted facilities should take in preparation, as well as how best to navigate implementation and compliance issues that may arise during the transition to mandatory smoke-free ORs.
West Virginia, Virginia and Minnesota join the ranks of 15 other states that have passed similar laws to date: Arizona, California, Colorado, Connecticut, Georgia, Illinois, Kentucky, Louisiana, Missouri, New Jersey, New York, Ohio, Oregon, Rhode Island and Washington. Two of these states’ laws were passed in 2023, but went into effect this year: Arizona on July 1 and Ohio on Oct. 1.
Notably, both Democratic and Republican governors and legislatures have passed these laws, which shows that surgical smoke evacuation doesn’t appear to be a partisan issue.
The 2024 legislative landscape still holds slight promise that three additional states — Massachusetts, North Carolina and Pennsylvania — could pass similar surgical smoke evacuation laws to the 18 that already have. AORN Associate Director of Government Affairs Jennifer Pennock expects renewed efforts to get bills passed in those states (if necessary) and others in 2025.
If your state still hasn’t passed a smoke evacuation law and you’d like to get involved in the push to permanently evacuate smoke in its ORs, visit AORN Government Affairs for more information. AORN also offers resources that can help you develop and promote your facility’s own smoke evacuation policies — mandate or not.
— Joe Paone
JRMC’s decision to take matters into its own hands is a terrific example of perioperative leaders and staff affecting positive change from the ground up — working proactively without a mandate from executives or a state law in place to back them up. Its surgical team organized and built a strong case to clear surgical smoke from its ORs.
“Just keep firm in your beliefs,” advises Ms. Miller. “If this is something you want, and if you need to get buy-in with your surgeons, start looking for videos and get them the statistics. Once they see those statistics, I would hope that would change their mind. There’s a lot of good equipment out there. They can find whatever they need.” OSM
As the leader, you may need to communicate bad news to your team as changes or situations occur....
ASC leaders face many challenges in 2025 and increasing revenues will certainly be one of them....
In a modern workplace where change often comes quickly and relentlessly, a leader should embody the concept of learning to embrace an agile mindset....