- Home
- Special Editions
- Article
Creating a Top-Performing Sterile Processing Department
By: Jared Bilski | Editor-in-Chief
Published: 5/17/2023
The recipe for success is qualified staff armed with instrument-tracking technology.
A safe and efficient sterile processing department is a cornerstone of every facility’s infection prevention and safety efforts. Top-tier SPDs almost always rely on a two-pronged approach to peak performance: a combination of qualified staff and proven technology.
Let’s look at how that combination works in tandem to keep up with the demand high-volume facilities face each day.
A pipeline of qualified candidates
First and foremost, you need to put the right team of SPD technicians in place to ensure the critical task of reprocessing instruments and assembling trays is performed in a safe and efficient manner — and keep that department adequately staffed. That’s no easy task, according to William Bryant, DNP, MBA, RN, NE-BC, CNOR, vice president of perioperative services at ChristianaCare. Dr. Bryant says the highly competitive market and a demand for flexibility are making it exceedingly difficult for SPD leaders to attract and retain top talent. “Market demand is really tilting the hand of many qualified candidates,” he says. “I think the other major factor is flexibility of work shifts. Long gone are the traditional ‘five eights.’ People want ‘four 10s’ or ‘three 12s’ or even ‘five fours’ for people returning to work.”
Accurate, adequate staffing models are a must if you want to keep your SPD running like a well-oiled machine. “Staffing models that don’t account for the ‘what if’ scenarios — leaves, vacancies, volume surges or depreciation — can put people in a bind and leave SPDs feeling like they don’t have an adequately staffed model of care to support the procedural or unit demand,” says Dr. Bryant, adding that in many cases staffing models only look at ideal situations instead of accounting for constant fluctuations. “You can use historical performance to say, ‘At any point in time, we have a 15% vacancy, 10% of our staff is going to call off, we need 2% of an FTE committed for educational purposes,’ and all the variables that happen,” he says. “But often we don’t fully account for these variables and then we wonder why we don’t have enough people or why we have too many people.”
The best way to overcome the staffing challenges described above? By keeping a well-stocked pipeline of qualified candidates filled and ready to step in. ChristianaCare does this through an in-house intern program that attracts qualified candidates — regardless of whether they have direct SPD knowledge — and places them in an intensive six-month program that, when completed, leads to a minimum one-year contract in its sterile processing department. “It consists of 200 hours of coursework, where interns go through the book to prep for the exam for the certification, and then they do another 400 hours of hands-on didactic training in the department, so they understand the flow and actually get relevant SPD experience,” says Wendy Carbonara, BS, CRCST, CHL, CIR, CER, ChristianaCare’s sterile processing director and the head of its SPD internship program.
Staffing models that don’t account for the ‘what if’ scenarios — leaves, vacancies, volume surges or depreciation — can put people in a bind and leave SPDs feeling like they don’t have an adequately staffed model of care to support the procedural or unit demand.
William Bryant, DNP, MBA, RN, NE-BC, CNOR
The program, which is entering its fifth year, ensures the SPD is always staffed to process the broad spectrum of instrumentation it handles. Ms. Carbonara’s advice for other facilities on the fence about creating their own intern program: It’s absolutely worth it. “It’s a large undertaking to do it, but we always have an inflow of candidates coming through that we can use to fill spots if they’re vacant,” she says. “Ultimately, our SPD makes sure that everyone understands what needs to be done and what goals need to be met, and they have proper tools and supplies to do those things in adequate time.”
What you need, when you need it
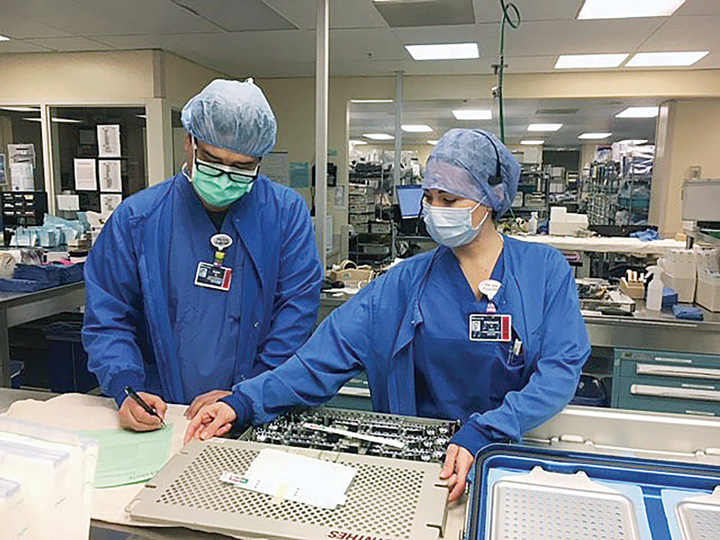
A well-staffed department filled with talented, experienced technicians is only part of the recipe for a top-performing SPD. You also need to equip your staff with the right tools to get the job done efficiently and expediently. That’s why most SPD leaders swear by instrument-tracking systems that can tell you exactly where your instrument trays are in the reprocessing journey at any given time.
Jig Patel, ST, CRCST, CHL, CIS, CER, sterile processing educator/quality assurance manager for UCLA Health offers a scenario that happened to him recently as just one of the many examples of how valuable these systems can be to facilities in terms of digging deeper. “We had these two trays where the picture in the system [the tracking system allows users to upload photos] wasn’t matching up with what was on the count sheet,” he says. “I went to update the picture and that’s when I realized there were some questionable things, and I reached out to the nurse who was in charge of that service line.” By reaching out, Mr. Patel discovered the nurse rarely used the trays in question. That prompted him to send the nurse the usage report and all the information he has on those instrument trays — reporting info that’s easily accessible through the system itself — over the past two years and, lo and behold, those two trays had only been used 16 times over the course of the past two and a half years. “When I communicate with certain folks outside of SPD, I can give them a lot of information to sort of pre-answer any of their questions thanks to the instrument-tracking technology,” says Mr. Patel.
Depending on the type of instrument-tracking system your facility invests in, SPD leaders and technicians can quickly locate items needed for urgent, time-sensitive procedures in the OR, adjust their inventory management practices by tracking usage of instruments for purchasing, create efficiency reports and easily spot maintenance issues. The latter can prove especially beneficial when you’re leading an SPD at a high-volume facility. “We do a ton of transplants, and every 10 uses you want to do a sharpening of the scissors or any cutting instrumentation,” says Mr. Patel. “If a transplant surgeon says, ‘Our instruments are always dull,’ I can easily run the usage report and find out if we’re using the instruments more than anticipated.” From there, Mr. Patel can adjust the preventive maintenance from, say, 10 uses down to five or take a more proactive approach to purchasing backups.
SPD leaders often find themselves pressured to get new hires onboarded and performing at peak efficiency as quickly as possible, an area in which these systems can definitely help. “If you have a new hire and you compare instrument-tracking technology to a paper count sheet, the tracking system will help staff learn more quickly and effectively,” says Mr. Patel. “For example, you need your new staff to learn certain trays, and if you associate photos with each of the individual instruments during training — items they may never have seen before — your new hires are learning the instruments as they go instead of just reading the items off of the count sheet.”
While this technology is generally standard for larger health systems, even small ASCs with razor-thin margins can benefit from instrument-tracking systems. “I believe this type of system pays for itself in terms of eliminating waste, the time you spend looking for instrumentation,” says Mr. Patel. “You can easily track when the instrument was last scanned and the location, which also adds a safety component.”
Blueprint for success
As SPD leaders everywhere can attest, there is a blueprint for lasting success in this critical area of care. If you look under the hood of the top-performing sterile processing departments, chances are you’ll find a well-trained team of technicians, a fruitful pipeline of qualified candidates and cutting-edge technology. OSM
.svg?sfvrsn=be606e78_3)
.svg?sfvrsn=56b2f850_5)