West Virginia and Virginia clear the air in their ORs.
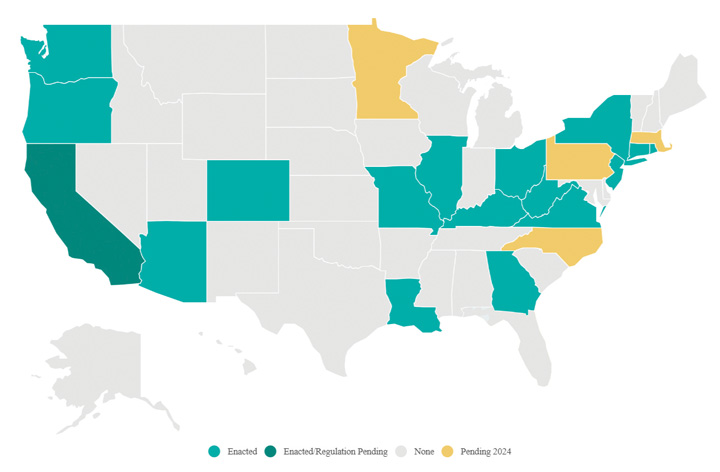 GOING GREEN As of May 2024, the 17 states in green have passed surgical smoke evacuation laws, while the four states in yellow remain in play for possible votes this year. | AORN
GOING GREEN As of May 2024, the 17 states in green have passed surgical smoke evacuation laws, while the four states in yellow remain in play for possible votes this year. | AORN
More than a third of U.S. states have now mandated the use of smoke evacuation systems in ORs, as West Virginia became the 16th state and Virginia the 17th to enact such legislation.
On Mar. 22, the Mountain State’s Republican governor, Jim Justice, signed HB 4376 into law. The Association of periOperative Registered Nurses (AORN), which has worked tirelessly in all 50 states to help advance smoke evacuation legislation, reports the new law will require West Virginia’s Office of the Inspector General to propose rules for legislative approval that will require a healthcare facility to utilize a smoke evacuation system during any procedure likely to generate surgical smoke. Any health facility subsequently in violation will be subject to a fine of $1,000 to $5,000 per violation. The law goes into effect on Jan. 1, 2025.
Surgical smoke evacuation advocates credit the efforts of W.Va. Delegate Phil Mallow (R-Marion) in getting HB 4376 over the finish line. "Delegate Mallow has championed the issue of surgical smoke evacuation since he first introduced legislation in 2022," says Dawn Yost, MSN, RN, CNOR, CSSM, manager of surgical support services at WVU Medicine in Morgantown and AORN’s West Virginia State Council Chair. "We are grateful for his advocacy and persistence and look forward to January 1, 2025, when all facilities will need to evacuate surgical smoke."
In Virginia, the commonwealth’s House and Senate passed identical bills: HB 763 and SB 537, respectively. Both were signed into law by Republican Gov. Glenn Youngkin on Mar. 28. Virginia’s law goes into effect on July 1, 2025, which gives surgical facilities in the state more than a year to prepare.
The development of the law was a grassroots effort. Janet Shortt, MHSA, BS, RN, CNOR, president of AORN Chapter 4702 in Richmond, engaged the Virginia Nurses Association about the importance of surgical smoke evacuation. The organization agreed and added surgical smoke evacuation legislation to its 2024 policy agenda.
Ms. Shortt offered a public comment on HB 763. "After 20 years in the OR, after three bouts of bronchitis and multiple upper respiratory infections, I was diagnosed with asthma," she said. "I thought this odd as I was living a healthy lifestyle, working out five days a week and eating a healthy diet. I now have chronic asthma that requires inhalers." She said surgical smoke aggravates her asthma and makes her eyes water.
In fall 2023, AORN surveyed its members in Virginia to gauge the availability and usage of surgical smoke evacuation equipment in the state. The good news: 94% of respondents said their facility had smoke evacuation equipment. The bad news: Only 26% said that surgical smoke was always evacuated during smoke-generating procedures. These results helped drive home to legislators the necessity of a mandate to ensure that surgical smoke evacuation systems are not just present at facilities but actually used for every smoke-generating surgery.
West Virginia and Virginia join the ranks of 15 other states that have passed similar laws to date: Arizona, California, Colorado, Connecticut, Georgia, Illinois, Kentucky, Louisiana, Missouri, New Jersey, New York, Ohio, Oregon, Rhode Island and Washington. According to AORN, bills for the 2024 session currently remain under consideration by legislators in four states: Massachusetts, Minnesota, North Carolina and Pennsylvania.
To get involved in surgical smoke evacuation advocacy in your state — or to arm yourself with resources to develop and promote smoke evacuation policies at your own individual facility — visit AORN Government Affairs for more information.
.svg?sfvrsn=be606e78_3)



.svg?sfvrsn=56b2f850_5)