Three nurses perform a study to better understand and mitigate surgical smoke exposure among pediatric patients.
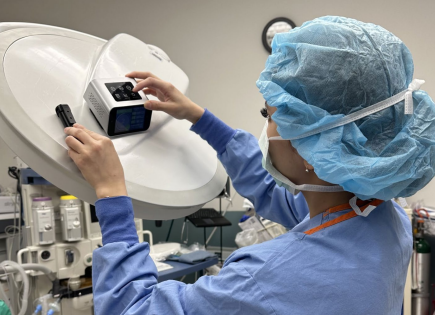 MEASURING POLLUTANTS During the study, the nurses placed calibrated monitors near the surgical field, as shown here, and other areas to gather data on contaminant levels during smoke-generating pediatric procedures. | Nancy Do, Andrea Dyer, Megan Nolan
MEASURING POLLUTANTS During the study, the nurses placed calibrated monitors near the surgical field, as shown here, and other areas to gather data on contaminant levels during smoke-generating pediatric procedures. | Nancy Do, Andrea Dyer, Megan Nolan
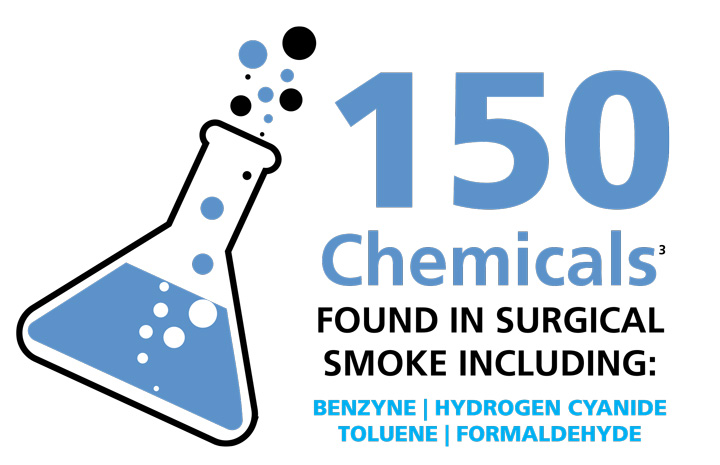
We’ve long heard about the dangers of surgical smoke exposure and how it can threaten the long-term health of staff and patients in the OR, but what about its impact on the youngest patients — those undergoing pediatric surgeries?
Three nurses affiliated with Boston Children’s Hospital and Harvard Medical School Teaching Hospital — Nancy Do, BSN, RN; Andrea Dyer, MSN, RN, CNOR; and Megan Nolan, MSN, RN, CNOR, NEA-B — performed a pilot study to investigate the issue, the results of which they submitted as a poster at the 2024 Association of periOperative Registered Nurses (AORN) Global Surgical Conference & Expo in Nashville. "By evaluating the efficacy of smoke evacuation systems in pediatric surgical settings, we aim to enhance safety measures for both patients and healthcare providers," wrote the nurses. "Despite growing awareness of this issue, effective mitigation strategies specifically tailored to pediatric cases are lacking."
The nurses’ pilot study assessed the effectiveness of a smoke evacuation unit attached to an electrocautery device in reducing levels of hazardous pollutants during pediatric spinal and hip procedures. The nurses measured carbon monoxide (CO), formaldehyde, total volatile organic compounds (VOCs) and particle counts during pediatric spinal and hip procedures using calibrated monitors placed near the surgical field and the anesthesia station. Regular suction was employed in both arms of the study to remove additional smoke, and data from the first hour of each case was included in a statistical analysis.
The nurses then compared pollutant levels between procedures with and without the use of a smoke evacuation unit attached to the electrocautery device. The differences were stark, with contaminant levels significantly reduced when smoke evacuation was employed:
- CO was measured 27 parts per million without smoke evacuation, but just 2.5 parts per million with smoke evacuation — a 90.7% decrease.
- Formaldehyde was measured at 0.698 milligrams per cubic meter without smoke evacuation, but just 0.151 milligrams per cubic meter with smoke evacuation — a 78.4% decrease.
- Total VOCs were measured at 0.515 milligrams per cubic meter without smoke evacuation but just 0.0175 milligrams per cubic meter with smoke evacuation — a 96.6% decrease.
- Particle counts were measured at 362 micrograms per cubic meter without smoke evacuation, but just 160.5 micrograms per cubic meter with smoke evacuation — a 55.7% decrease.
Beyond the obvious conclusion given those numbers that smoke evacuation systems should be present and activated during smoke-generating pediatric surgeries, the nurses identified additional areas for improvement. They encourage perioperative nurses to advocate for patient safety, especially by promoting the adoption of best practices in smoke evacuation. They also call for greater awareness and more training among perioperative nurses about the risks associated with surgical smoke exposure to empower them to help create safer perioperative environments for pediatric patients.
The nurses concluded that their pilot study "highlights the need for ongoing research and innovation to further optimize smoke evacuation strategies and improve patient outcomes in pediatric surgery."
.svg?sfvrsn=be606e78_3)


.svg?sfvrsn=56b2f850_5)