- Home
- Article
What’s New in Smoke Evacuation?
By: Carina Stanton | Contributing Editor
Published: 5/8/2023
With 11 states requiring smoke-free ORs and 10 more considering it, now is the time to act by sharing the evidence and securing C-suite buy-in.
In the past five years, a flood of literature on surgical smoke hazards has confirmed what nurses and surgeons have been complaining about and, in extreme cases, even dying from for years — surgical smoke transmits toxins, carcinogens, viruses and other particles directly through masks into the respiratory system of anyone in the OR.
Hurdles and challenges
The reality of surgical smoke hazards hasn’t been lost on the periop professionals who are increasingly choosing employment in smoke-free ORs. It has also caught the attention of a growing number of legislators passing laws to require smoke evacuation, according to Jennifer Pennock, associate director of AORN Government Affairs. Ms. Pennock works directly with perioperative and other legislative professionals to advocate for legal smoke evacuation protections at the state and federal level.
Despite solid evidence, challenges exist in the logistics of purchasing smoke evacuation equipment, modifying workflows to ensure safe and consistent use, and making sure surgeons feel comfortable using the technology.
“Sometimes starting an active conversation around smoke evacuation can be one of your greatest hurdles,” notes Jamie Nelson, MBA, BSN, RN, CPHQ, CSSGB. As manager of quality and clinical projects for surgical services, she helped lead a large-scale project at Memorial Hermann-Texas Medical Center in Houston to successfully launch a smoke evacuation initiative across 47 ORs. Initial discussion of the project fueled few questions and little feedback with the facility’s Surgeon’s Council Steering Committee and at each of the surgical service line meetings. This changed once Ms. Nelson partnered with vendors to have smoke-free cautery pencils and compatible cautery tips available to view, touch and try. “This was key to jumpstarting the dialogue with the surgeons,” she says. “I don’t think the surgeons knew what to ask until they had the opportunity to participate in show-and-tell.”
To secure C-suite approval to purchase evacuation equipment, gathering clear numbers on the cost of evacuation equipment and associated consumables such as tubing and filters can help make your case. A detailed implementation plan for using the technology can also be helpful to get the green light for purchasing. “Some facilities that have achieved smoke-free status found it beneficial to conduct a product evaluation with a representative from every team to ensure the smoke evacuation purchase provides the best value for team needs,” says Hannah Campbell, project and program specialist for AORN’s Center of Excellence in Surgical Safety. Ms. Campbell has worked with more than 272 healthcare facilities who have received the Go Clear Award for achieving and sustaining smoke-free ORs through AORN’s Center of Excellence in Surgical Safety: Smoke Evacuation. The program provides teams with a structured process to educate staff and implement smoke evacuation practices.
Speaking firsthand from their respective roles in achieving smoke-free ORs, Ms. Pennock, Ms. Campbell and Ms. Nelson share their perspectives on the current climate for going smoke-free and the resources to clear the air in any operative setting.
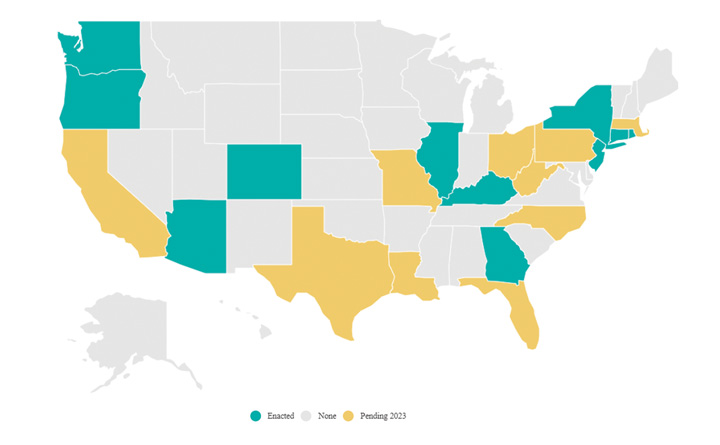
Since 2018 when the first smoke evacuation requirement was passed in Rhode Island, many other states have followed suit. The best place to track the current status of enacted and pending smoke evacuation laws is through AORN’s National Map of Current Surgical Smoke Evacuation Laws and Legislation at aorn.org/get-involved/government-affairs/policy-agenda/surgical-smoke-free-or/smoke-bills.
As states continue to adopt smoke evacuation, Ms. Pennock said most of these state laws allow facilities plenty of time to develop their policies, educate staff and purchase any needed equipment. “If a bill is introduced in your state, you don’t need to wait for a governor’s signature to begin the process of complying with the provisions of the bill,” she advised. “Perioperative teams can get ahead of any coming requirements by trialing smoke evacuation products and educating staff on the changes that will be put into place.”
— Carina Stanton
Status check on legislation
For almost a decade, AORN has been working on surgical smoke evacuation legislation across the country that would require facilities, including ASCs, to adopt and implement policies to ensure that harmful surgical smoke is evacuated for the health and safety of OR staff and patients. To date, 11 states have put smoke evacuation laws in place, including Arizona, Colorado, Connecticut, Georgia, Illinois, Kentucky, New York, Oregon, Rhode Island, Washington and New Jersey — the newest state to pass legislation. From 2021 to 2023 alone, nine of these state laws passed, suggesting a trend in this legislation, according to Ms. Pennock.
She says increased concerns about air quality and transmission of the SARS CoV-2 virus that causes COVID-19 may be one reason for a surge in laws. With viruses such as human papilloma virus (HPV) known to be transmitted via surgical smoke from patient to staff, researchers have suggested COVID-19 could also be transmitted this way. Broader concerns about OR air quality have also called into question how surgical smoke particles could enter an incision and increase the risk of surgical site infection.
Selling smoke-free
Whether your state requires smoke evacuation or not, the climate around this issue suggests it will likely become a more widespread practice. Here are some common strategies that have helped facilities of all sizes successfully achieve smoke-free ORs.
• Secure champions with the ‘whys.’ Sharing the facts on surgical smoke hazards can win buy-in from OR team representatives to support the broader effort. For example, a well-cited study by Hill et al quantified the mutagenicity of surgical smoke to be as harmful as smoking 27-30 unfiltered cigarettes per day, increasing the risk of cancer and neurodegenerative diseases.
A 2019 review by Liu et al discussed cases of the same types of HPV lesions excised during surgery as the cause of surgeons and nurses in the room developing laryngeal cancers. These are the types of studies discussed in the Go Clear Award education modules that demonstrate the risks associated with occupational exposure to surgical smoke.
• Share a cost/benefit analysis with the C-suite. Convincing your C-suite leaders that the upfront investment in smoke evacuation is well worth it in the long run requires a data-driven approach. Engaging in collaborative product evaluation with materials management can help confirm the upfront cost of evacuation equipment as well as long-term expenses for filters, tubing and other smoke evacuation components that will need to be replaced.
In addition to sharing detailed numbers on the actual cost of the equipment, it can be beneficial to discuss the costs of not evacuating surgical smoke, such as for team members requiring medical care for acute and chronic conditions such as chronic obstructive pulmonary disease (COPD) resulting from surgical smoke exposure. For example, a 2021 study by Xie et al found that nurses who worked in the OR for 15 years or more had a 69% greater risk of developing COPD compared with those who never worked in an OR.
ASC nurses and leadership may also want to evaluate the cost of onboarding and training new periop nurses because staff working in facilities that do not evacuate often leave for facilities that consistently do evacuate surgical smoke (or choose to work in states that already have an evacuation law), notes Ms. Pennock. “With healthcare staff retention such a big issue and major concern with policy makers and stakeholders, the cost of not evacuating surgical smoke is too great when ASCs are competing for staff in a tight job market.”
• Make smoke evacuation a familiar safety tool. Help OR staff feel confident with using smoke evacuation technology efficiently in their workflow by including their input in policy and procedure documents. Important elements of the documents should include procedural interventions such as how to position the smoke capture device and how to safely handle used smoke evacuation parts such as tubing and filters with standard precautions as biohazardous waste. Before officially implementing a smoke evacuation program, Ms. Campbell says “teams have gotten creative with opportunities for all team members to handle smoke evacuation equipment, even making time for a lunch-and-learn or setting up equipment in the staff lounge.”
• Collaborate with smoke evacuation technology reps. It can prove invaluable to trial smoke evacuation equipment, so users have a chance to test-drive it and have a say in which technology is selected. Once a product is selected, or if the facility already has purchased smoke evacuation technology, inviting a rep to walk through usage in detail can help teams ask questions that will help them use the technology on a daily basis.
• Listen and validate concerns with evacuation technology. An historic barrier to becoming smoke-free for many facilities has been pushback from surgeons. Often this concern stems from poor experiences with smoke evacuation in the past, as well as issues with how using the technology can negatively impact workflow and create delays. In certain cases, such as using a smoke-free cautery pencil in delicate and confined surgical spaces, surgeons may have valid concerns about visibility and pressure injury to the patient.
For example, pediatric surgeons at Ms. Nelson’s facility have not found a way to adapt to the smoke-free cautery pencils. However, the project has centered around a two-pronged approach using in-line smoke filters for suction canisters and use of smoke-free cautery pencils with smoke evacuation devices, so the in-line suction filter would still be used for those surgeons who are unable to use the smoke-free cautery pencils, she says. “We have also suggested the manufacturer develop a smoke evacuation handpiece that would work with our smoke evacuation machines, would not be mistaken for regular suction and would not be dependent on activation of a cautery pencil.” OSM
When implementing a plan for smoke-free ORs, leverage existing data and proven strategies from others to win over leadership and your frontline. Start with these resources to help build a successful argument:
• AORN Guideline for Surgical Smoke Safety. This scientific and data-driven resource confirms the necessity for surgical smoke evacuation to protect OR staff health. An updated version of the guideline was published in October 2021 with new studies and an even greater emphasis on team-wide involvement in the smoke safety plan.
• AORN Management of Surgical Smoke Tool Kit. This collection of tools provides shareable clinical resources to assist with staff education and awareness, including a presentation discussing the components of a smoke evacuation system and how to handle them properly in different situations such as for minimally invasive surgery.
• AORN Go Clear Award. Facilities can seek recognition for becoming smoke-free by registering for free to participate in the AORN Center of Excellence for Surgical Safety: Smoke Evacuation program to earn the Go Clear Award. The program includes required milestones and specific resources such as a gap analysis tool, education modules and product evaluation to help achieve smoke-free ORs.
• AORN Journal. A quick search on “smoke-free” will provide several articles sharing first-hand experiences and strategies from perioperative teams who have achieved smoke-free ORs.
— Carina Stanton
.svg?sfvrsn=be606e78_3)
.svg?sfvrsn=56b2f850_5)