Procedural issues, inconsistent counting processes and fearful staff can lead to damaging results.
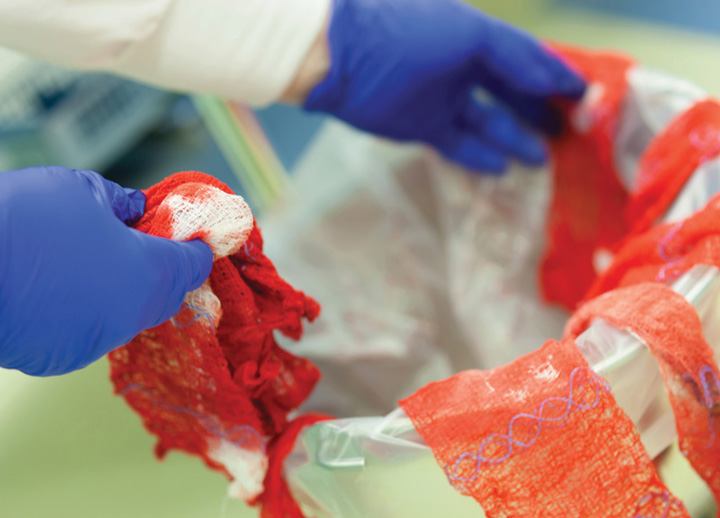 NO SPONGE LEFT BEHIND The importance of removing every object from every patient before wound closure is a laborious but vital aspect of patient safety.
NO SPONGE LEFT BEHIND The importance of removing every object from every patient before wound closure is a laborious but vital aspect of patient safety.
There were 88 unintended retained surgical item (RSI) events reported to The Joint Commission (TJC) in 2022, continuing a downward trend established in 2019, when 144 were reported. Still, RSIs remain one of the most prevalent sentinel events in surgery, and Lisa DiBlasi Moorehead, EdD, MSN, RN, CENP, CPPS, CJCP, field director of TJC’s hospital/psychiatric hospital pro¬gram and accreditation and certification operations, says the reasons are usually multifactorial.
"It’s generally some combination of a having a difficult procedure, an inconsistent counting process and a culture in which members of a perioperative team don’t feel comfortable speaking up if they think something might be wrong," she says.
Procedural flags. Dr. Moorehead says higher risks for RSIs are present when operating on patients with high BMIs, during emergency procedures, when an unanticipated clinical change takes place mid-procedure, when a patient undergoes more than one procedure at a time, when a patient is being treated by more than one surgical team, or when a staff turnover takes place during a lengthy surgery.
Inconsistent counting process. "As surveyors, we try to be in the OR as the room is being prepared so we can observe the count to see if they’re using a highly reliable process," says Dr. Moorehead. "As we’ve seen again and again, any consistent process that a facility puts in place is an effective mitigation strategy against human error."
Fearful staff. Dr. Moorehead says RSI risks grow when OR staff doesn’t feel comfortable enough to say something when the count seems off, and stresses the need to establish a culture of safety in such organizations. "You need to encourage people to speak up and, when they do, put strategies in place to make sure they’ll do so again," she says. Leaders should act on information staff provides, then thank the employee for bringing it to their attention and inform them that not only was action taken, but the fact that they spoke up made a positive impact.
This is especially important, she says, because only about 2% of RSI events are self-reported to TJC, often due to fear of lawsuits or being located in states where peer reviews aren’t protected. "Employees can’t fear retribution or feel intimidated in any way if they say something about what they saw, or they’ll never speak up the next time," says Dr. Moorehead. "Organizations should identify reporting barriers and do everything they can to eliminate them and simplify the reporting process wherever possible."
.svg?sfvrsn=be606e78_3)



.svg?sfvrsn=56b2f850_5)