- Home
- Article
Ready for an MH Crisis
By: Carina Stanton | Contributing Editor
Published: 10/19/2023
From promptly recognizing symptoms to implementing proper response protocols when every second counts, here’s how two surgical leaders are adequately (and creatively) preparing for malignant hyperthermia events.
Malignant hyperthermia (MH) is a rare hypermetabolic reaction a patient may have in response to a medication given during general anesthesia. It’s genetic, and patients likely won’t know they could have an MH reaction until it happens — no matter how old they are, where the surgery takes place or why they are in surgery. Without a rapid response to identify MH and administer dantrolene — the life-saving medication that reverses the reaction — a patient’s organs can fail, making it unlikely they will survive.
An entire career without incident
In such a high stakes scenario, a timely and coordinated response is key, but it’s not easy, explains Teeda Pinyavat, MD, associate professor of anesthesiology at Columbia University and the New York Presbyterian - Morgan Stanley Children’s Hospital of New York in New York City.
For one, MH is extremely rare. “An anesthesiologist may practice their entire career and never see it,” she says. MH is also challenging because it presents in different ways so “actually pulling the trigger to diagnose MH is not simple because the differential diagnosis is so broad.”
As medical director of the MH Hotline offered through the Malignant Hyperthermia Association of the United States (MHAUS), Dr. Pinyavat has helped many OR teams determine if a patient is experiencing MH. “High fever is the reason for many calls we get, but we’ve learned through MH research that high CO2 in the blood [hypercarbia] is the most frequent sign of an actual MH reaction.”
For example, she recently talked an anesthesiologist colleague through an actual MH reaction. “The patient presented with a slow rise in temperature and a fast spike in CO2 that could not be ventilated away,” says Dr. Pinyavat. “Due to the coordinated action of the anesthesiology, nursing and surgical teams, the crisis was treated quickly with dantrolene, and signs abated within minutes with no consequences to the patient.” She says even the most knowledgeable providers can benefit from calling the MH hotline and discussing the differential diagnosis when MH is suspected.

A 2021 study published by Dr. Pinyavat and colleagues in the Anesthesia Patient Safety Foundation newsletter shared these four key lessons learned from MH Hotline calls taken:
- Isolated postoperative or post-intubation hyperthermia is a poor predictor of a “likely MH” diagnosis by an expert consultant.
- Episodes arising in an operating room and those including hypercarbia as a clinical sign more often led to a “likely MH” consultant impression.
- Blood gas analysis is the most commonly recommended diagnostic test during a call.
- Dantrolene is commonly recommended by consultants, even when they are unsure of an MH diagnosis.
—Carina Stanton
Orchestrating a coordinated response
Once the MH diagnosis is made, the surgical team has only minutes to respond before life-threatening effects of MH progress. Rapid response can be even more challenging in an outpatient surgery center if dantrolene is not kept in stock. The complications of MH increase substantially for every 10-minute delay in treatment with dantrolene, with a 100% complication rate after 50 minutes, according to a 2014 study by Riazi et al.
Dr. Pinyavat stresses the importance of training and drills to help every member of the team feel confident in their role. “Without a coordinated response plan that is trained and retrained regularly, teams may stumble, losing valuable life-saving minutes to recover the patient,” she says.
She recommends in situ training, such as in the OR, using a crisis checklist that would be applied in an actual MH event so each team member can practice their respective roles together. “The trick is presenting the education in a way that will prepare every team member to remember what to do when they must respond immediately in the heightened stress of an actual MH crisis,” says Dr. Pinyavat. That’s exactly why Donna Hameier, RN, BSN, CNOR, perioperative services educator at CHI St. Luke’s - The Woodlands Hospital in Conroe, Texas, turned her MH education into an immersive game environment.
Without a coordinated response plan that is trained and retrained regularly, teams may stumble, losing valuable life-saving minutes to recover the patient.
Teeda Pinyavat, MD
Gamifying education to reinforce knowledge
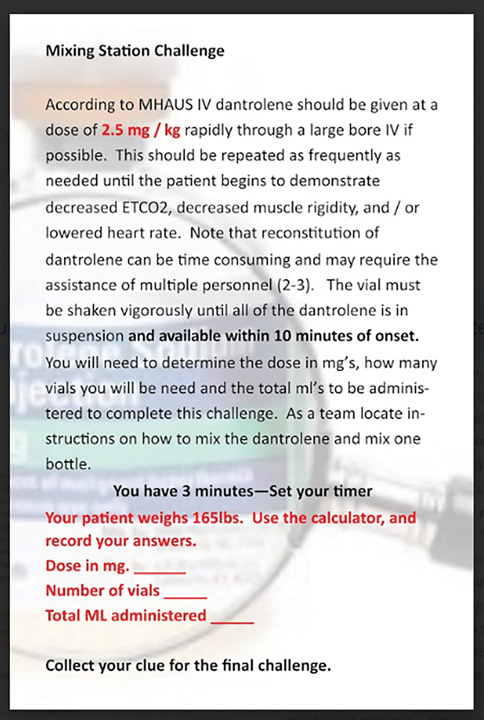
All perioperative professionals working in the seven ORs at Ms. Hameier’s facility fulfill their annual MH competency training through an escape room activity where escaping the OR depends on how well they can solve common MH challenges together, such as mixing dantrolene and knowing whom to call for help.
Gamification is an educational approach that presents non-game information through traditional game elements such as solving a problem as a team to encourage cooperation and strengthen relationships. “I wanted to create a learning experience that would provide participants with the necessary information to function efficiently during an MH crisis, stimulate an interest in learning, increase retention and provide measurable results,” says Ms. Hameier. While there was plenty of relevant literature on escape rooms being used in healthcare, she found very limited ideas for those specific to MH. This meant she had to get creative.
While presentation of MH can vary, there is one constant with MH response, according to MHAUS Executive Director Linda Scholl: When a member of the response team “recently had some MH training or did some reading on MH they were able to identify the symptoms and get the patient the help they needed.”
MHAUS offers these resources at mhaus.org to help teams better prepare for a safe, timely and effective MH response:
- MH Hotline (1-800-MH-HYPER) offers 24/7 access to a physician with substantial expertise in MH. When a care provider suspects an MH event is occurring, even if they are unsure, they can call the MH Hotline to get help determining if they are dealing with an MH event and how to treat the patient.
- MH Mock Drill Kit provides laminated task cards for each team member.
- MH Prep Check brings MH experts to offer a 60- to 90-minute training session that includes an MH readiness walk-through, on-site MH mock drill training and review of the facility’s specific plan to transfer an MH-susceptible patient.
- Faces of MH shares true stories of MH survivors and the quick responses that saved their lives.
—Carina Stanton
Choosing a large OR to serve as the escape room, she created an MH-specific patient scenario and designed challenge stations located strategically where actual MH response activities would take place for the patient. In small groups, her learners had to solve specific challenges, such as a word search to identify the symptoms of MH, a scavenger hunt to explore an MH crash cart to memorize the location of key supplies and a dantrolene mixing station where the team had to locate instructions and reconstitute dantrolene for their patient. She printed each challenge on a large poster. Solving a challenge resulted in a clue, and collecting a clue from each station gave learners the chance to exit the OR with a stable patient outcome.
After the first MH escape room education event, she surveyed learners and found that her gamble to gamify MH knowledge paid off. Her post-training survey showed 100% of her learners were highly satisfied with the education and more comfortable with what they need to do during a real MH situation. “I’ll be honest, this was the first time this type of learning modality was introduced to the staff,” says Ms. Hameier. “It required a lot of time to research, prepare and implement. I felt this could only go one of two ways; it would be a great success or a great failure. I was very pleased to see it was a success.” She attributes this significant success to three main approaches:
- Survey for specific learning needs. Using an online accessible pre-assessment survey to identify learning needs, Ms. Hameier developed specific objectives to support the identified learning gaps.
- Respect learners’ time. The MH escape room required a commitment of approximately 30 minutes for staff to complete.
- Make it fun. Having small groups competing to complete the challenges created a sense of urgency and engagement.
To reinforce learning throughout the year, staff are assigned MH e-learning modules and participate in an annual mock MH drill. Ms. Hameier is also planning new challenges for next year’s escape room to address knowledge gaps and keep it fun. OSM
.svg?sfvrsn=be606e78_3)
.svg?sfvrsn=56b2f850_5)