- Home
- Article
Photo Essay: Patient Positioning
By: Jennifer Parrott, RN
Published: 3/4/2024
A visual guide on a critical perioperative process.
Surgical positioning can be an undervalued task for all staff. They can and do perform this task several times throughout the day and but can lapse into autopilot mode.
Staff can perform this task without being attentive; however, positioning is one of the first steps performed within the operating room that demonstrates advocacy for that patient. The knowledge and skill that is required is imperative to protect the surgical patient from harm.
Throughout school and training, healthcare workers are presented with several intrinsic and extrinsic factors that must be considered upon positioning patients for surgery.
First and foremost, attention must be given to the type of surgery being performed and the exposure needed for that surgery. Once that is determined, careful consideration must be given to:
- type and length of procedure
- limited exposure for prevention of hypothermia
- ability to maintain correct anatomical alignment
- care and protection of bony prominences and tissue
- Age and weight, and
- Respiratory and circulatory safety.
It’s always a good practice to regularly review this crucial protocol. Let’s look at four commonly utilized patient positioning techniques within the operating room.
Supine
Supine positioning is one of the most common patient positions within the surgical setting. aWhen a patient is in the supine position, it means the patient is lying on their back with their face and torso pointing upward. Forethought and care must be taken to protect and support bony prominences such as their arms, coccyx and heels. Upon positioning the arms, they should not be extended more than 90°.
Improper support, or no support, can lead to tissue and nerve injuries. Unfortunately, the two most common types of injuries that can present themselves when patients are not positioned and/or supported correctly in the supine position are ulcers and damage to the ulnar nerve. In order to prevent injury, healthcare workers should use an approved mattress (polyurethane, gel, or memory foam) in conjunction with adjunct positioning aids such as gel or disposable foam.
Prone
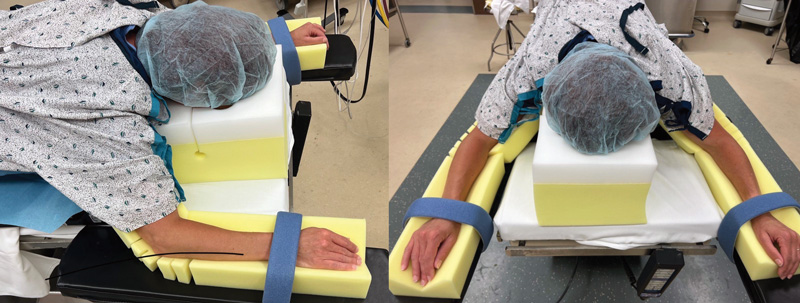
In the prone position, the patient patient is oriented with the face and torso down.
In order to accomplish this, however, a prone supportive device is a necessity. These can include chest rolls, foam positioners, Wilson frames and other types of tools.
Care must be taken to protect all bony prominences, tissue and nerves; however, a major safety factor when utilizing this position is in the care of the head. Healthcare workers should utilize a head positioner with padding with particular attention paid to the eyes, nose and ears. When weight or pressure is applied to the cartilage areas, there is risk of a hematoma forming, ischemia or necrosis.
Beach chair

This position is a common position in the world of shoulder arthroscopies and total shoulder arthroplasties.
The patient is placed into a sitting or reclining position, elevated from 30-90°, with the head being supported by a device. The healthcare worker must take care and be especially attentive to the head and neck area. The head positioner supports the patient’s head and is secured firmly but comfortably to the patient’s head and face with Velcro straps. The headrest itself is curved on the sides to prevent pressure aon the ears.
Care must be taken to protect the patient’s eyes from corneal abrasions and lacerations. Preferably, a disposable eye protector is ideal.
Lateral
This positioning entails rolling up a patient onto their side, called side-lying, with the operative side exposed.
Pillows are placed between the patient’s flexed legs to prevent tissue injury to the legs, knees, heels and feet.

The pillows prevent injury to the hip by preventing adduction or internal rotation. There are several lateral positioning devices available, such as a bean bag, hip grip, Montreal positioner or peg board.
The main positioning device is imperative; however, it doesn’t stop there. Many adjunct devices are critical to ensure proper care and support for the patient. These include but are not limited to: pillows, axillary, rolls, lateral support head positioners, arm boards, foam and gel pads. All of these devices work together to ensure the patient is in proper anatomical alignment to prevent skin breakdown, nerve injuries, and proper respiration.
Final thoughts on an often underappreciated task
Every worker in the healthcare field takes an oath to do no harm to their patients. Sometimes it pays to step back and look at practices that become second nature over time.
If you are not taking the necessary time to position your patients correctly, you are causing harm to them. If you do not have the support devices needed, please speak up and remember the importance of advocating for the safety of your patients. Always ask yourself, “If this was my loved one, or myself, would this be right?”
At the end of the day, remember this timeless piece of advice: These are people who are trusting in you to care for them, and you are their advocate. OSM
.svg?sfvrsn=be606e78_3)
.svg?sfvrsn=56b2f850_5)