- Home
- Article
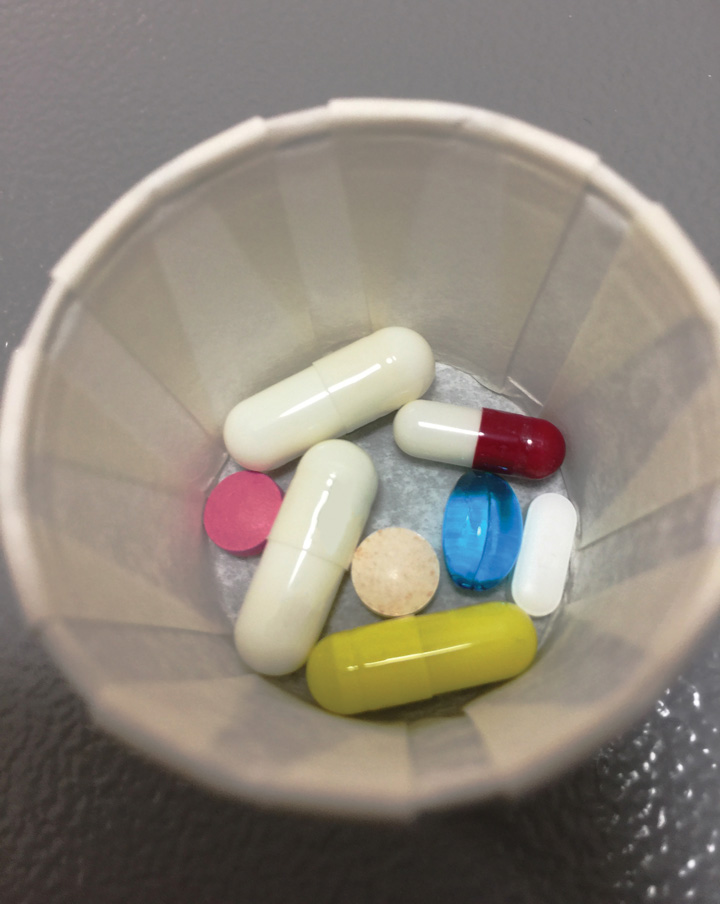
Multimodal Pain Management Made Easy
By: Kendal Kloiber | Contributing Editor
Published: 4/5/2023
Take orthopedic procedures to the next level using these opioid-sparing, recovery-expediting techniques.
Multimodal pain management has a domino effect on surgical outcomes: By using this approach, facilities reduce opioid use, which often translates into less post-op nausea, a quicker discharge and recovery, and overall greater patient satisfaction.
Plus, by relying less on addictive narcotics as a quick fix for pain, multimodal analgesia is an important step in reducing the risk of long-term opioid abuse by patients.
Prevent pain from the get-go
An approach that Kern Singh, MD, professor in the department of orthopedic surgery and co-director of the Minimally Invasive Spine Institute at RUSH University in Chicago, swears by for his patients — including for his outpatient cervical disc replacement cases — is preemptively tackling their pain before they ever set foot in the OR. “The belief is that, if we can prevent pain from the beginning, we can decrease it overall,” says Dr. Singh. “We deliver medication as soon as the patient is in the holding area.”
That regimen includes giving patients an anti-inflammatory, a muscle relaxer and a tablet of hydrocodone soon after they check in for surgery. This approach has led to his patients requiring fewer narcotics and medications intraoperatively, which leads to fewer cases of post-op nausea and less “playing catch-up” to try to reduce a patient’s pain postoperatively. “We saw a revolutionary change by delivering the medications before surgery and before they even entered into the holding area,” says Dr. Singh. “It allows those medications to get into the bloodstream and start working.”
Target pain pathways
When a patient undergoes surgery, there are several factors in play that cause them to feel pain. Opioids only treat a select few of those pain pathways. “If you stub your toe, it’s painful and often the first thing you do is reach down and rub it, which floods the bad pain signals with good ones,” says Dr. Singh as an example. “You could technically treat it with a heavy dose of narcotics, or you could treat it with a little Bengay and/or an anti-inflammatory medication.”
Merging the idea of what is causing the pain and how to approach it is what led to the effectiveness of multimodal regimens, says Edward R. Mariano, MD, MAS, FASA, professor and senior vice chair of the department of anesthesiology at Stanford (Calif.) University School of Medicine. “For example, you start with a source of pain, like a surgical incision for a knee replacement,” explains Dr. Mariano, who also serves as section chair for education and research for the American Society of Anesthesiologists. That incision, he says, creates local inflammation, and that inflammation causes pain that’s transmitted by the nerves from the site of pain to the spinal cord, to the brain — and all are targets for pain management therapies.
Both Dr. Singh and Dr. Mariano stress the importance of customization. “A true multimodal approach isn’t throwing everything we have at the patient,” says Dr. Mariano. “It’s tailoring pain management for the individual patient by targeting multiple different sites.” Dr. Mariano notes that those who receive spinal anesthesia for elective joint replacement typically have a much more pain-free recovery after surgery, and there are fewer instances of confusion or prolonged emergence, which can sometimes delay early activity.
For patients who experience severe post-op pain, Dr. Mariano says that intravenous opioids may be administered as needed. For the opioid-tolerant patient who receives general anesthesia, consider intraoperative low-dose ketamine infusion. Surgeons can also perform local infiltration analgesia before the end of the case, which can be especially effective if used in combination with continuous nerve blocks.
“Regional nerve blocks are not available everywhere, but I wish they were,” says Dr. Mariano. “If you have the skillset where regional or peripheral blocks are an option, then that’s the way to go. If not, then local anesthetic infiltration around the joint is also effective. In truth, infiltration by the surgeon alongside nerve blocks works even better together.”
Postoperatively, patients can use old-fashioned ice and elevation, as well as take a multimodal approach to their medications, which may include a combination of acetaminophen, anti-inflammatory medications and, for the first few days, small amounts of opioids. “We know that combining certain elements of multimodal pain management works well,” says Dr. Mariano. “We also know that when there are no contraindications, acetaminophen and NSAIDs are effective when used in combination and are opioid-sparing.”
Realistic, expectation-setting education
To implement a multimodal approach, it’s critical to thoroughly educate your patients on what to expect in terms of pain. At Dr. Singh’s facility, he walks his cervical disc replacement patients through how their pain will be treated, how the medications work and why they’re going to be giving them specific treatments in great detail. By handling a patient’s anxiety on the front end, they are more likely to feel safe and prepared for the post-op reality.
“When patients hear ‘low dose,’ they worry they’re going to be in pain, but almost all of my patients wake up and say it was a phenomenal experience,” says Dr. Singh.
Education must include realistic expectation-setting, understanding what normal pain trajectory is, and what medications the patient will be taking and why. Developing this protocol with your surgeons and surgeons’ offices is key, according to Dr. Mariano. “I think that developing a protocol should involve providing common education for patients and caregivers,” he says. “When the patient shows up on the day of surgery, the nurses who bring in their pre-op oral analgesics can say this is part of the pain management plan that’s been introduced to them. It’s much less stressful when the plan has been established by everyone and expectations are set ahead of time.”
The importance of patient education is backed by research. In a study co-authored by Dr. Mariano, patients undergoing knee arthroplasty were given a more comprehensive pain scale to use when describing their pain to providers. The scale provided specific information on what a 7 means versus a 10, as well as a description and viewing of faces of pain for additional clarity.
Patients also received a full, written list of their medications, with details and information on what the medications were, when they would be taking them and how they could receive or ask for them. After introducing these two educational interventions, the study’s authors saw inpatient opioid usage decrease. “It’s a great example of how patients being participants in their own care can help us provide them with better care,” says Dr. Mariano. “You have to leverage your entire team, with the patient as part of that team.”
Edward R. Mariano, MD, MAS, FASA, professor and senior vice chair of the department of anesthesiology at Stanford University School of Medicine and section chair for education and research for the American Society of Anesthesiologists (ASA) is a major proponent of multimodal protocols. In a study on multimodal pain management for total joint procedures, he and his co-authors even offer a sample regimen for total knee patients that includes these preoperative measures (after counseling on expected pain and thorough medical assessment):
• Acetaminophen 1000 mg and celecoxib 400 mg by mouth (in no contraindications).
• Insert an adductor canal catheter under ultrasound guidance in the regional induction area (“block room”); add infiltration between the popliteal artery and capsule of the knee (IPACK) block if the surgeon does not routinely perform local infiltration analgesia at the end of surgery.
• If applicable, continue chronic analgesics on the day of surgery and postoperatively.
• For the chronic pain or opioid-tolerant patient, consider giving a single dose of gabapentin 300-600 mg by mouth (lower dose in elderly and renal insufficiency).
—Kendal Kloiber
Opioids’ limited role
Opioids have traditionally been the go-to for many orthopedic cases, but because they don’t treat every pain pathway, they aren’t 100% effective and patients often must continue to increase the dose to get the desired effect, says Dr. Singh. “If you can instead control the pain pre-, intra- and postoperatively instead, the patients are less sedated afterward, there’s less constipation, and we see a faster recovery.”
That doesn’t mean opioids should be banished from the entire pain-control protocol, though. Instead, it’s important to find the right dose, the right number of tablets, and have a weaning plan in place, says Dr. Mariano. In another study he co-authored on tailoring opioid use to be patient specific and include a weaning plan, researchers found that multidisciplinary implementation of an opioid prescribing and tapering protocol at discharge decreases the total dose of opioid prescribed by 63% for a six-week period after total hip arthroplasty.
At Dr. Mariano’s facility, the day after surgery, scheduled and intravenous opioids are discontinued for almost all total hip cases. Using each patient’s prior 24-hour opioid consumption, the prescribing physician, nurse practitioner or physician assistant will write the discharge opioid script using a tailored approach that includes weaning info. For instance, a patient who consumed 30 mg of oxycodone 24 hours before discharge will start with a maximum daily dose of 30 mg for Days 1 and 2 after discharge. This will decrease to a max daily dose of 20 mg for Days 3 and 4, and just 10 mg for Days 5 and 6. “Our goal is opioid-sparing, for those instances when there is severe pain preventing mobility,” says Dr. Mariano. “They are an important class of medications for pain management, but they’re not the only class.”
By taking a multimodal, opioid-sparing approach, surgeons like Dr. Singh can take procedures that were once inpatient-only — such as cervical disc replacement — and now have patients home in time for lunch. “I performed several surgeries today, and it’s 1 p.m. now, and they’re all going home,” says Dr. Singh. “By using this approach, we can avoid narcotics, avoid addiction and treat pain just as effectively.” OSM
.svg?sfvrsn=be606e78_3)
.svg?sfvrsn=56b2f850_5)