- Home
- Article
Is It Time to Outsource Your Revenue Cycle Management?
By: Carina Stanton | Contributing Editor
Published: 6/27/2024
Experts share when and how an outside firm can help, while also providing tips on how best to keep it all in-house.
Is your volume up? Are you adding a new service line such as cardiology with more complex coding? If the demands of revenue cycle management (RCM) are stretching your team thin, software capabilities and partial outsourcing options could help.
Don’t be too quick to partner with just anyone, though, cautions Jessica Nelson, vice president of revenue cycle services for Surgical Information Systems (SIS), which offers web-based ASC management solutions, revenue cycle services and analytics for outpatient care services.
And make sure to maintain a close connection with your billing activities no matter if you outsource or if you keep RCM in-house, advises Shakeel Ahmed, MD, MRCP, FACP, FACG, FASGE, an interventional gastroenterologist, surgeon and CEO of Atlas Surgical Group, one of the largest ASC and ancillary services networks in the Midwest.
Ms. Nelson and Dr. Ahmed recently shared insights from their respective vantage points on optimizing RCM in the interest of helping ASC leaders make more informed decisions to maintain their centers’ financial health.
Revenue functions frequently outsourced

It takes skilled coders to prevent denials and skilled billers to ensure prompt reimbursement. On the patient side, a solid system for educating patients about their financial responsibilities is needed, along with an equally strong system for presurgical insurance verification. If an ASC falls behind in any of these areas, costly gaps in lost revenue can quickly snowball, says Ms. Nelson.
To help ASCs overcome such challenges, SIS offers a range of services through all phases of the revenue cycle, primarily serving independently-owned ASCs. The company provides a wide array of services, including coding, billing, following up after claims denials and patient collections. Coding is the primary service SIS performs for ASCs, as many facilities choose to handle most of their revenue cycle duties themselves. SIS estimates that about 20% of surgical facilities opt to have a company handle all of their RCM work, while about 17% opt for partial outsourcing arrangements.
Dr. Ahmed advocates for this hybrid model if internal resources are stretched thin when the complexity of billing and compliance exceeds the capabilities of your staff, or when the cost of maintaining an in-house team outweighs the outsourcing expense.
However, even when outsourcing parts of RCM, an internal oversight committee that works hand-in-hand with the external team is needed, he says. For a mid-sized business, this in-house team should include an experienced coder, at least two data entry clerks, two or three billers and RCM experts, and a billing manager and coordinator.
This committee should meticulously track all data entries and postings. “We recommend the ‘numbers in, numbers out’ formula, meaning the team should reconcile the number of patients seen and surgeries performed daily with the number of bills coded and submitted,” says Dr. Ahmed. He suggests the committee meet daily and engage external billers at least weekly.
What to look for in an outside firm
“Any outsourcing company you partner with should offer transparency through open lines of communication, data sharing and analysis,” says Ms. Nelson. “The more data and insights you get from your outsourcing partner, the more insights you have to bring back to your physicians and owners.” As an ASC shops for external RCM support, Ms. Nelson suggests asking these questions to find your best fit:
Any outsourcing company you partner with should offer transparency through open lines of communication, data sharing and analysis.
Jessica Nelson
• Will we share a software platform? Get the details on how the external company will connect with your clinical scheduling and registration system. Using the same technology as your outsourcing partner is a great opportunity to uncover opportunities for automating workflows, such as for billing.
“If they are working through the same system, it can be much more effective,” says Ms. Nelson. “Otherwise, there could be a lot of handoffs outside of the system that could create lost visibility in understanding the status of patient outcomes.”
• When will you share data? Physicians and owners will want quick access to accounts receivables data. That’s why the exchange of this type of information must be fluid between the center and the outside company. “This is where leveraging outsourcing support can be very valuable because a center might not have the internal bandwidth to track and analyze data regularly, but external support must provide that data quickly,” says Ms. Nelson.
• How much will the services cost? Price obviously is a huge consideration for an ASC looking to outsource. Ms. Nelson suggests making sure you compare apples to apples with services offered. “Remember that a lower rate doesn’t necessarily equate to quality of service,” she says. “Some outsourcing companies can offer lower prices because they may not be offering the same service or are offshoring certain functions. Visibility and transparency will help you understand the services’ pricing models to make informed decisions.”
• How will you coordinate with our internal liaison? When you outsource, you need an internal expert to manage the relationship. For example, if your external partner identifies trends in denials that require a change in physician documentation, or they need to speak with your materials manager about an implant’s price missing from a claim, these issues need to be resolved quickly to prevent costly delays.
It’s also important to understand the broader communication processes to expect, including how often will you connect and what information you will have access to, says Ms. Nelson. “Your outsourcing partner should feel like an extension of your business operations that you can connect with as quickly as walking to another office, whether through email or videoconferencing as often as needed,” she says.
Tips to optimize Your revenue cycle internally
Dr. Ahmed prefers to keep RCM functions across the multiple centers that comprise Atlas Surgical Group in-house. There is nothing more productive than a hands-on team that knows the intricacies of your business,” he says.
While larger outside billing companies excel at coding, billing and pursuing your money efficiently, they often neglect smaller amounts and typically focus on easy collections, says Dr. Ahmed. He refers to these third parties as “one-click experts,” meaning they prioritize funds that come in with the first submission or appeal and lose interest afterward. ”In-house billing teams, on the other hand, are dedicated solely to your practice and will pursue every dollar because they are not managing multiple accounts simultaneously,” he says. “This singular dedication ensures thorough and persistent efforts in maximizing revenue collections for your business.”
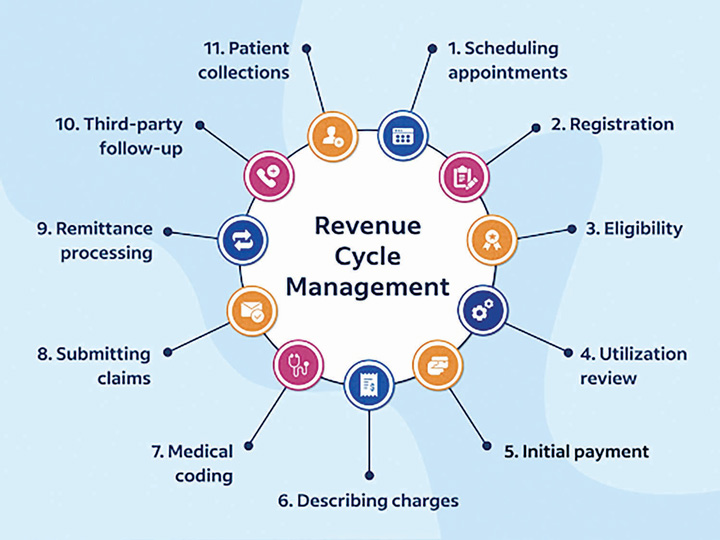
While the services of RCM providers vary, generally these companies will handle the following functions:
- Certified coding
- Pre-service verification
- Charge entry
- Billing
- Payment posting
- AR follow-up
- Denials management, and
- Patient collections.
—Carina Stanton
Dr. Ahmed suggests your in-house RCM staff incorporate the following strategies:
1. Delegate administrative tasks. Train team members to lead patient billing and claims processing. Dr. Ahmed’s team members regularly participate in seminars and training courses to remain proficient in the latest billing and coding techniques. “This ensures our practices are both current and effective,” he says.
2. Consider automation. Look for opportunities in your RCM software to automate tasks such as billing. “This can save staff time for more complex tasks such as adequate coding to help reduce denials and get reimbursed more expediently,” says Dr. Ahmed.
3. Prioritize analytics. By integrating practice analytical tools at all of its facilities, Atlas is able to monitor billing and coding trends in the industry and adjust accordingly. For example, the group uses metrics to compare receivables and payments to ensure all possible payments are captured. “If there is a sudden non-payment of an ancillary code for surgery by insurance companies, we will adjust our billing practices accordingly,” says Dr. Ahmed.
4. Review and renegotiate payor contracts. Keep a close eye on any potential updates with payor contracts to prevent underpayments and ensure you’re operating under the most favorable terms possible, says Dr. Ahmed. “We reach out to insurance companies to request higher payments for surgeries that our centers perform and are currently paid at higher rates to local hospitals,” he says. “This strategy typically captures their attention.”
5. Bridge the gap between billing and patient care. Because billing is deeply intertwined with patient care, Atlas integrates its billing team into aspects of patient management. Dr. Ahmed says this approach provides a nuanced perspective on the intricacies involved. “I regularly engage in detailed discussions about surgeries and procedures with our billers, because it enhances their ability to navigate the billing process with greater precision and effectiveness,” he says. OSM
.svg?sfvrsn=be606e78_3)
.svg?sfvrsn=56b2f850_5)