- Home
- Article
Investing in Big Screens Could Mean Big Outcomes
By: Adam Taylor | Senior Editor
Published: 10/10/2023
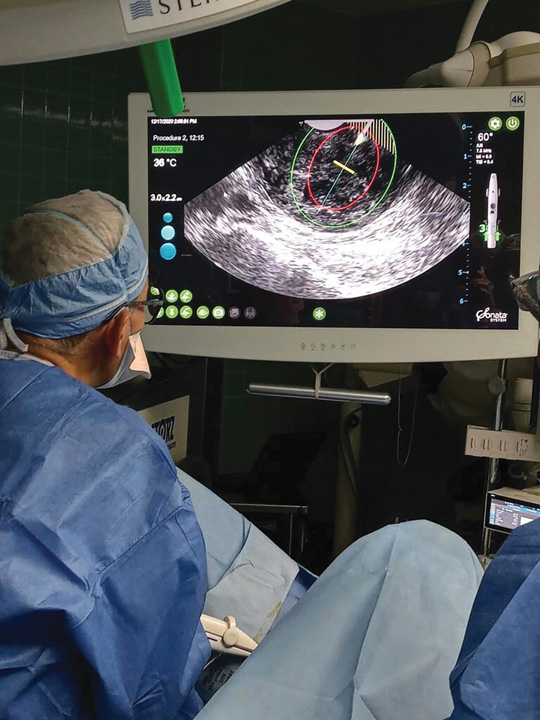
4K ultra high-definition imaging systems provide optimal lighting, color and resolution so surgeons can be more precise.
If a patient with a small shoulder wound would have been seen by surgeon J. Gabriel Horneff III, MD, FAAOS, earlier in his career when he was armed with 1K imaging systems with small monitors, chances are he wouldn’t have been able to see it.
Now that Dr. Horneff and other surgeons have 4K ultra high-definition imaging systems with huge monitors at their disposal, they certainly can.
Better than ever
In addition to identifying smaller issues that could have been missed, being able to see crucial anatomy in finer detail and clarity allows surgeons to make repairs with more precision and with better results.
“I would have been able to see a large rotator cuff tear or possibly even a small labrum tear with the old technology,” says Dr. Horneff, assistant professor of shoulder and elbow surgery at the University of Pennsylvania in Philadelphia. “But if a patient said they were in pain, they could have had a very small tear, and everything would have looked fine on an old-style monitor.”
• Big screens. The size of the monitors — on which the heightened quality of the images generated by the 4K cameras appear — is a big part of the appeal. They allow surgeons to see images in greater detail because of the high refresh rates and very small pixels that drive the technology. “Just like the TVs in our houses, we now have flatscreen monitors we use for arthroscopy on the walls instead of having a smaller monitor attached to a big clunky tower,” says Dr. Horneff. “The images are delivered wirelessly to the monitors, so it makes for a cleaner and safer operating room in general.”
This can be especially helpful in older operating rooms “in which every inch of square footage is precious territory,” notes Dr. Horneff. “Some new operating rooms are enormous, but some of the older ones essentially only have room for the OR table and for the staff to stand. A wall monitor can free that room up to be used for different types of cases that couldn’t be performed in it simply because it was so small.”
Some designers and planners of new and renovated ORs note that bigger isn’t always better, especially if there’s an OR team who prefers multiple displays in the sterile field. Additionally, there are also super-sized wall screens in some hybrid ORs that can be used to project several separate images in mini boxes on the large screen. This allows a team to watch different aspects of the case on the same screen at the same time.
This enhances teamwork and makes for efficient, timely cases, as all perioperative team members are seeing the same images. In these instances, there is often a single 4K display near the surgeons for use when they want to view the main high-resolution image in an instant.
Of course, there’s no such thing as a “4K monitor.” Buying a 4K monitor attached to a 1K imaging system might make for a slightly better picture, but certainly nothing like what a true 4K system provides. In fact, a new monitor only would roughly equate to having the clarity of an HDTV at home. The entire 4K chain includes multi-chip camera heads and image-enhancing algorithms that brighten dark areas of images so surgeons, using color contrasts, can make real-time distinctions between different parts of a patient’s anatomy. It’s essentially a GPS system that can tell the surgeons where they are and where they should go. It’s best if the monitors used are from the same manufacturer as the rest of the imaging chain rather than mixing and matching components.
These systems that locate, identify and brighten dark areas of an image in real time assist surgeons so they don’t need to increase brightness levels or move scopes closer to see the dark areas. The technology also different tissue structures so surgeons can make instant distinctions between blood vessels and other parts of the anatomy by using color contrasts.
• Detailed images. The 4K technology has a high sensitivity to view fine details and the sharper images it delivers to the larger screens allows surgeons such as Dr. Horneff to identify smaller tears and smaller fissures of cartilage that they might not have with the old technology, simply because they would have been blurred out by the limited reproduction abilities. “I wouldn’t be able to appreciate the smaller injuries because the detail in the resolution of the image wasn’t as good,” notes the surgeon. “Before, I might not have even been able to see it, but now I can and can address it.”
The increased clarity of 4K images displayed on big screens not only makes for better diagnoses, but it improves surgeon performance as well. “Using this technology and instrumentation arthroscopically makes for more precise placement of sutures and anchors,” says Dr. Horneff. “The difference is as if someone were operating in an open field but wasn’t wearing the corrective lenses they’d been prescribed.”
4K systems enhance the trained eyes of surgeons and allow them to see tissue, droplets and polyps that might have otherwise gone undetected. The increased depth perception they get during arthroscopic and laparoscopic procedures makes them better able to see blood vessels and visualize tissue planes, which reduces unintended nicks and decreases blood loss during procedures. It also makes for less trauma, lower levels of post-op pain, shorter recovery times and faster safe discharges.
• Advanced applications. There is even the ability to use green light fluorescence to highlight structures of the body to make them more visible for surgeons. This is done by injecting indocyanine green (ICG), which allows surgeons to toggle back and forth between the traditional white lighting and the fluorescent imaging with the green contrasting agent. Its advocates say surgeons use the technique to make better decisions and to ID structures they need to avoid during the case in order to prevent patient injury. It can be used during gall bladder surgery, colon procedures and bowel resections.
Dr. Horneff notes the value of 4K-quality images will be a must during procedures that involve integrating and overlapping images, enhancement software, or those that use augmented reality headsets. Starting that integrative process with a comparatively blurry 2K image wouldn’t work as well.
• 4K now and into the future. The technology is most widely applicable to outpatient settings affiliated with large health systems due to the price. That is expected to change over time, as price points drop and younger physicians, and eventually patients, will begin to demand it. And even though 8K technology is emerging, it’s not a threat to 4K’s relevance. 8K technology’s prominence is years away, as planners note that imaging systems, microscopes and other devices are still catching up to 4K, so 4K is still the technology to consider for at least the next few years.
“The difference we have in our operating rooms now is similar to how our home televisions have improved over the years,” says Dr. Horneff. “What we have with our arthroscopy towers and the monitors that are attached to them or on the wall is life-like in comparison.” OSM
.svg?sfvrsn=be606e78_3)
.svg?sfvrsn=56b2f850_5)