- Home
- Article
Guest Editor: Bringing It All Together
By: Maureen Spencer, M.Ed., BSN, RN, CIC, FAPIC, and Peter Graves, BSN, RN, CNOR
Published: 4/23/2024
Keeping patients safe from infection requires dedication to evidence-based guidelines and facility-wide collaboration.
As inpatient procedures continue to shift to outpatient surgery centers, the need for heightened SSI prevention strategies, implementation, monitoring and collaboration between infection preventionists and OR teams is more important than ever.
In this Outpatient Surgery Magazine Special Edition: Infection Control, you’ll find information on the latest in skin prep and nasal decolonization techniques, quick-but-safe room turnover strategies, and the latest on surface and whole-room disinfection. You’ll also learn about more effective SSI-reducing bundles. This is critical information to have when you consider some of the alarming findings about SSIs:
• In 2015, U.S. hospitals reported more than 110,000 SSIs associated with inpatient surgeries. The exact number of SSIs in outpatient centers, however, is more challenging to determine due to specialization, settings and inconsistent reporting practices.
• Patients with an SSI are five times more likely to be readmitted after discharge, twice as likely to spend time in the ICU and twice more likely to die after surgery.
• If a patient is infected with Methicillin-resistant Staphylococcus aureus (MRSA), the risk of death increases twelvefold.
• At $3.3 billion annually, SSIs are the costliest of all healthcare-related infections in the U.S.
Following published infection control guidelines can significantly reduce the incidence of SSIs. It is crucial to implement infection control practices and measures that are evidence-based to improve outcomes and reduce the cost burden of SSIs. The good news is that an array of evidence-based infection control and prevention guidelines are available from reputable organizations such as AORN, American College of Surgeons, Surgical Infection Society, CDC, WHO and state health departments.
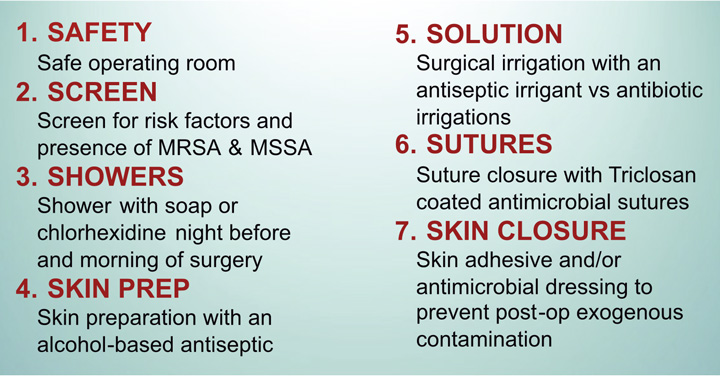
One evidence-based strategy that can be used in the development of your own SSI prevention program is the 7S bundle (See graphic). Facilities can follow the 7S framework exactly or customize it to fit their own needs. In addition to the 7S bundle, infection preventionists and surgical services should incorporate recommendations from the guidelines we listed when developing and implementing their SSI prevention bundles.
A multidisciplinary approach to infection control is vital. Each department brings unique abilities, perspectives and skill sets that, together, can better guarantee comprehensive, effective and safe care for surgical patients. Infection prevention specialists and surgical services leaders can often provide guidance on best practices and protocols. Healthcare quality professionals can monitor patient outcomes and identify areas for improvement. Medical technology experts can advise on the latest tools and equipment to reduce the risk of SSIs, while facility administrators can allocate resources and support staff training. Environmental services play an often-underappreciated role in supporting a clean and sterile surgical environment. Together, we can make quality patient care better and safer.
Surgical stewardship teams can develop and implement lasting comprehensive SSI prevention bundles. Facility-wide collaboration ensures a more comprehensive approach to patient care, leading to better patient safety, satisfaction and outcomes. OSM
.svg?sfvrsn=be606e78_3)
.svg?sfvrsn=56b2f850_5)