- Home
- Article
Four Ways to Stop Sharps Injuries Cold
By: Carina Stanton | Contributing Editor
Published: 9/30/2024
A team commitment to sharps safety, sound reporting and consistent use of engineered safety tools all play a role.
If you haven’t had a sharps injury, you might be less inclined to speak up when you are directly handed a used sharp on the sterile field. What’s the big deal, right? Wrong. While a poke or cut from a used sharp could simply perforate a glove or even require a few stitches, the actual harm is potential exposure to a deadly bloodborne disease like HIV or hepatitis that can require lifelong treatment and lead to chronic health conditions. Sharps injuries can also put a patient at risk for disease transmission from an injured provider when an injury occurs inside the operative site.
Unfortunately, a lack of consistent focus on sharps safety in all perioperative settings is putting OR teams and their patients at risk.
Sharps injuries on the rise
Despite seemingly increased awareness and prevention efforts, needlesticks and other sharps injuries are actually up 16% from 10 years ago, with 42.8% of needlestick and sharp object injuries occurring in ORs in 2023, according to surveillance data from the International Safety Center’s EPINet.
“The highest percentages of injuries and exposures occur in the operating room and PACU, most often from devices being used in a multi-step procedure like passing,” explains Amber Hogan Mitchell, DrPH, MPH, president and executive director of the International Safety Center. Beyond the OR, indirect exposure across the perioperative setting can be just as dangerous. Sterile processing professionals and environmental services staff are at risk for exposure when a sharp is not properly packaged for reprocessing or disposed of correctly.
“These same risks transfer to outpatient surgery centers, yet usually without full support of a health and safety or infection prevention team,” notes Dr. Mitchell.
A “matter of action”
Known in the healthcare community as the “needlestick lady,” Dr. Mitchell speaks from experience as a former industrial hygienist for OSHA, a researcher in occupational infection disease, and an advocate for sharps safety practices. “We’re much past the ‘awareness’ level on occupational exposures to bloodborne and infectious disease in perioperative settings,” she says. “We accept the risk to be true. Now, it’s a matter of action.”
Dr. Mitchell and other experts working in and beyond the perioperative setting expressed this need for action in a 2020 consensus statement, Moving the Sharps Safety in Healthcare Agenda Forward in the United States. The statement was timed with the 20th anniversary of the Needlestick Safety and Prevention Act, which had appeared to spur reduced sharps injuries in the short-term. Unfortunately, says Dr. Mitchell, that sharps safety momentum hasn’t been sustained.
Amanda Heitman, BSN, RN, CNOR, agrees that sharps safety efforts must be elevated to a national level. After experiencing a sharps injury early in her career, she now works on numerous fronts to advocate for sharps safety practices, including as a clinical educator and through her perioperative educational consultancy Periop Anew.
“While we recognize the risks working with sharps in surgical care, we must master the strategies that are well-established to reduce those risks,” says Ms. Heitman.
Team sport
A bundled approach is the best option for reducing the chance for a sharps injury to occur. However, Ms. Heitman and Dr. Mitchell agree that bundles are most effective when they are implemented within a culture of safety — a working environment where the importance of sharps injury prevention is recognized across the entire organization, no matter how large or small.
Here are four essential bundle elements they suggest as part of a tailored and comprehensive approach to reduce sharps safety risks in perioperative settings.
1. Establish an organizational sharps safety plan. Inconsistency in adhering to correct practices is a major barrier to effective sharps safety, says Ms. Heitman. Providers may have learned about using a neutral passing zone in their schooling, but a preceptor might describe a different approach or de-emphasize this important practice. This inconsistent education can lead students to mistakenly believe that a neutral passing zone is more of an extra precaution than a best practice.
Another consideration is that sharps safety training is inconsistent across various perioperative roles among an OR team. In other words, different members of the team may have different understandings of sharps safety best practices. This can be especially problematic in terms of using engineered sharps safety devices correctly and consistently. That’s why, in Dr. Mitchell’s words, “an organization-wide sharps safety plan is the kingpin of safety culture” because it provides a rare opportunity to standardize proactices while engaging and discussing the issue among all stakeholders.
In an outpatient setting, Dr. Mitchell suggests these stakeholders include representatives from each frontline perioperative role, center administrators, physician leaders and anyone with experience in infection prevention and occupational safety.
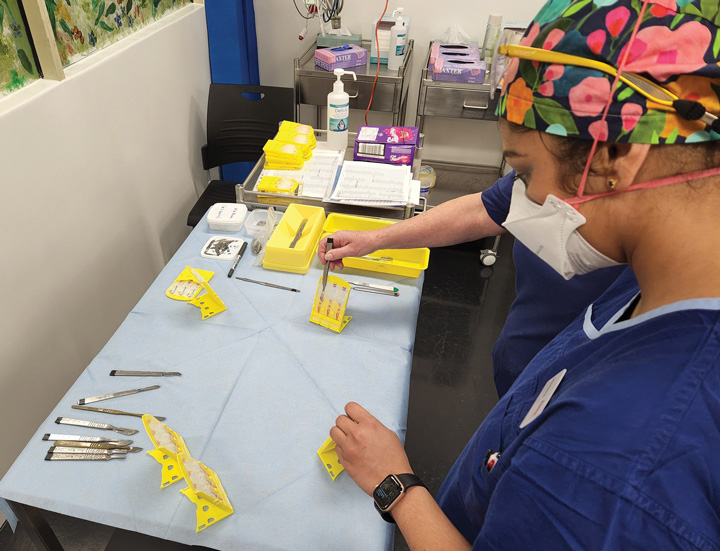
2. Select team-approved safety-engineered devices and PPE. “Sharps safety is most effective when using safety-engineered devices along with PPE and a neutral zone,” says Ms. Heitman. “All team members should test and select products to get buy-in for consistent use.”
To achieve this, she suggests setting up a quality improvement project that targets one or more key types of sharps safety devices to research, trial and test. One example is to review blade removal safety devices, including a single-handed scalpel blade removal device, which OSHA recently clarified as an engineering control. “The goal is to select a safety product that team members will champion because they chose it and because it functions optimally in practice,” she says.
New evidence on increasing the effectiveness of a sharps safety plan is highlighted in AORN’s soon-to-be published update to its Guideline for Sharps Safety, according to update lead author and sharps safety expert Emily Jones, MSN, RN, CNOR, NPD-BC.
Ms. Jones shares these critical steps from the guideline update that can improve your organization’s sharps safety plan.
Build a sharps safety team that includes those with authority. Perioperative leaders, frontline users and non-direct users indirectly impacted by sharps safety devices should be part of the interdisciplinary team that provides input into a sharps safety plan. Those with the authority to implement and support sharps safety practices, including physicians, should be part of this interdisciplinary team.
Put time into cultivating a culture of sharps safety. This level of engagement and cooperation is present when the following elements of a sharps safety plan are standard practice:
- Every team member adheres to all elements of the CDC/NIOSH hierarchy of controls for sharps safety.
- Prevention practices are standard when any sharp is used.
- Sharps injury reporting is simple to complete and encouraged.
Standardize sharps safety practices. Facilities that employ a bundled sharps safety approach that is ingrained in policy and procedure are more likely to experience fewer injuries. Here are some safety practices to include:
- Double glove when scrubbed.
- Use sharps with engineered injury prevention features.
- Implement a neutral zone.
- Use clear communication when passing sharps.
Refine injury reporting. Research shows that complete and accurate sharps injury reporting is important for injury follow-up and supports continuous quality improvement. Target barriers to reporting by looking at time constraints with complex reports and a lack of support to make a report, especially in the OR.
AORN’s updated Guideline for Sharps Safety will publish electronically at aornguidelines.org and in print in the 2025 edition of Guidelines for Perioperative Practice.
— Carina Stanton
3. Educate and re-educate with evidence and personal stories. Sharps safety devices alone will not protect staff from occupational injury if policy/procedure and education/training aren’t in place to guide teams on correct and consistent use. This is why Ms. Heitman tailors her OR education to cover device use along with correct application of PPE such as double gloving. “We discuss communication for how to use safety devices and PPE correctly, especially when a sharp is being passed from one provider to another,” she says. She also stresses the safety benefits of minimizing distractions, and not rushing.
Her education combines practical experience with explaining the evidence-based rationale for why consistent safety practices are essential. She covers OSHA requirements, evidence-based practices recommended by AORN and other professional practice organizations, and specific organizational policies and procedures.
She also talks about failures in safe practice that led to actual injuries in her experience.
“Sharps injuries happen far more frequently than we acknowledge,” says Ms. Heitman. “When we tell our own stories, it helps colleagues realize the risk for injury is very real for them, too.”
4. Improve sharps injury reporting. It can be difficult for many facilities to truly grasp the scope of the sharps safety problems in their own work settings due to spotty reporting of sharps injuries. Ms. Heitman says about half of all sharps injuries aren’t reported industrywide.
Dr. Mitchell notes that reporting is required by OSHA as part of the Bloodborne Pathogens Standard Exposure Control Plan and Sharps Injury Log. She recommends a stronger focus on non-punitive reporting of all needlesticks, sharps injuries and mucocutaneous exposure incidents, especially among physicians. Ensure that your staff isn’t afraid to report injuries for fear of punishment. OSM

Dr. Mitchell is pulling together a virtual stakeholder meeting to identify if and how the healthcare community needs occupational blood and body fluid exposure surveillance through The International Safety Center’s EPINet free surveillance database. A lack of funding is putting the center at risk of shuttering its doors. The 90-minute virtual summit will feature an expert panel followed by full attendee participation in “fireside chats” to set the national stage for the future. To participate in the meeting, email Dr. Mitchell at [email protected].
— Carina Stanton
.svg?sfvrsn=be606e78_3)
.svg?sfvrsn=56b2f850_5)