- Home
- Article
Do HOPDs Deserve Higher Reimbursements Than ASCs?
By: Adam Taylor | Managing Editor
Published: 3/3/2025
Independent ASCs bemoan getting less money than hospital outpatient departments for the same cases. Health systems claim the dichotomy is justified.
Hospital outpatient departments (HOPDs) feel they’re being nicked financially from all directions, which could continue to result in the provision of less medical care to needy patients that extends well beyond elective surgery.
Site-neutral payment debate
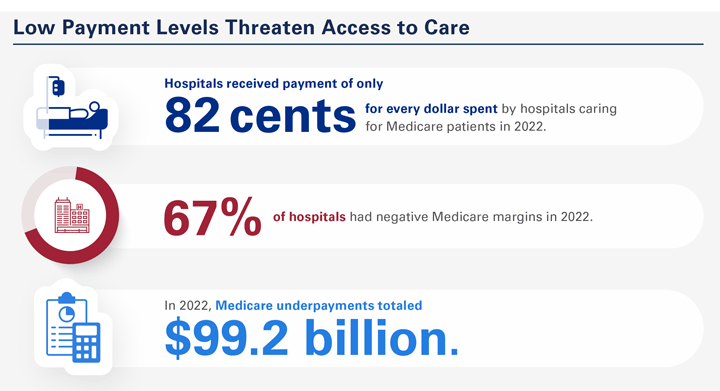
Hospitals are already underpaid for patient care across the board, according to the American Hospital Association (AHA.) That structural reimbursement crisis would only get worse if more site-neutral payment policies are enacted to allow ambulatory surgery centers (ASCs) to be paid the same higher amount of money HOPDs receive for performing identical procedures.
“Hospitals have a higher cost structure than independent physician offices (IPOs) and ASCs due in part to the costs of standby capability and capacity,” says the AHA. “This standby role is built into the cost structure of hospitals and supported by revenue from direct patient care — a situation that does not exist for any other type of provider.”
The AHA says there are several important reasons to oppose additional site-neutral payment proposals.
HOPDs and ASCs are not the same
HOPDs aren’t simply same-day surgical centers for health systems. They also provide complex cancer, infectious disease, mental health and other services — and therefore should not be paid the same Medicare rate as standalone physician offices.
“Implementing site-neutral payment policies could force outpatient clinics to close or cut back on critical services, resulting in reduced patient access and job losses,” notes the AHA. “The cost of care delivered in hospitals and health systems, including HOPDs, is fundamentally different than other sites of care and thus needs to take into account the unique benefits that only they provide to their communities.”
Those benefits include maintaining standby capacity for natural and man-made disasters, public health emergencies, other unexpected traumatic events and delivery of 24/7 emergency care to all who enter their doors, regardless of ability to pay or insurance status. “Since the hospital safety net and emergency standby roles are funded through the provision of all outpatient services, expanding site-neutral cuts to additional HOPDs and the outpatient services they provide would endanger the critical role that they play in their communities, including access to care for patients, especially the most medically complex,” states the AHA.
De facto rural primary care offices
Emergency rooms and HOPDs are often the first point of care for many low-income individuals from rural and urban areas. HOPDs also serve many older Americans. “The more rural the county that a Medicare beneficiary lives in, the more likely their visits take place in an HOPD rather than a physician office,” notes the AHA. A KNG Health Consulting report prepared for the AHA in 2023 showed that, from 2019 to 2021, HOPD patients had higher medical needs and were more likely to be low-income and/or minorities compared to those seen in ASCs and IPOs. They were also more likely to have been in an ER or had a hospital admission in the three months prior to their HOPD, ASC or IPO visit.
A study published on the JAMA Network showed that significant rural hospital closures have increased travel times for surgical patients.
Here are several prime examples why, in the eyes of the American Hospital Association (AHA), comparing reimbursement rates of HOPDs and ASCs isn’t as simple as declaring that identical procedures should get the same payment rate no matter where they are performed. These complex dynamics of HOPDs show it’s not an apples-to-apples comparison, according to AHA Policy Development Director Roslyne Schulman.
- Comprehensive services. HOPDs often provide a wider range of services, including specialized care, diagnostics and emergency care that independent physician offices may lack.
- Advanced equipment. HOPDs generally have access to more advanced medical technologies and equipment that can enhance quality of care and diagnostic accuracy.
- Collaboration with its hospital network. HOPDs benefit from being part of a larger health system, allowing for seamless coordination with inpatient care, specialists and other medical departments. Access to a variety of specialists within the same system can provide comprehensive care that may be harder to arrange at independent physician offices.
- Continuity of care. Patients can be easily referred to other hospital services such as inpatient care, often without needing to travel to a different facility. Further, many patients benefit from ongoing follow-up care in HOPDs, ensuring monitoring of chronic conditions or post-surgical recovery without an interruption of care.
- Regulatory oversight. Hospitals are subject to rigorous regulations and quality standards that can lead to high levels of safety and accountability.
- Community health hub. HOPDs can serve as a vital healthcare resource for local communities, especially in rural and other underserved areas, improving access to care for populations with fewer healthcare options.
- Shared electronic health records.The shared medical record within a hospital system positively impacts care for HOPD patients because it improves the flow of information, enhances communication and ultimately results in more coordinated, safer and higher-quality care for HOPD patients.
- Enhanced safety practices.HOPDs have practices such as decision support built into their sophisticated electronic health records systems, rigorous infection control practices that are implemented and emphasized by the infection control staff, and quality improvement activities that are launched by the hospital and evaluated by an accrediting body or other oversight agency.
—Adam Taylor
For the medically complex
A 2023 study shows HOPDs’ share of total joints arthroplasty appears safe, saying patients with health issues are getting their same-day hips, knees and shoulders done at HOPDs at a rising rate, while the rate for those patients at ASCs is declining. Nearly 12% of more than 222,000 shoulder and knee arthroscopies at HOPDs were performed on patients with high comorbidity rates, compared to less than 2% of 94,000 ASC patients. The study also found that unplanned hospital admissions following the procedures was lower for HOPDs than ASCs, although the stays were longer.
Shakeel Ahmed, MD, CEO of Atlas Surgical Group, with ASCs in Illinois and Missouri, says HOPDs would still make enough money if they only performed surgical procedures on patients with significant comorbidities. ASCs were created as a financial move, he notes, not just for facility owners, but to save the healthcare system significant money.
“We’re in this together — no ASCs can survive without hospital outpatient surgical departments simply because there is a subset of patients that can’t be serviced on an outpatient basis in an independent freestanding facility,” he says. “The reality is that we need each other. Sadly, my view is that only one side (the ASCs) seems to acknowledge that openly. The system actually pays quite well for complex surgeries. In a perfect world, all safer patients would move to outpatient settings. Money needs to take a backseat for hospital leaders’ priorities so that patients can get care in less expensive settings that would also help the country’s healthcare economy.” OSM
.svg?sfvrsn=be606e78_3)
.svg?sfvrsn=56b2f850_5)