- Home
- Article
Best Practices in Whole Room Disinfection
By: Benjamin D. Galvan, MLS(ASCP), CIC, CPH
Published: 5/16/2023
Evaluating your options to augment robust manual processes.
During the pandemic — and even before the arrival of COVID-19 — many healthcare facilities tapped into the high-tech power of whole room disinfection systems, such as ultraviolet (UV) light, hydrogen peroxide mist and visible light.
For specialists in infection prevention, it’s easy to make the pitch for whole room technology to supplement your manual cleaning processes and ensure another layer of protection to keep harmful pathogens out of the OR. In our role, we aim to do everything we can to ensure the safety of our facilities, our patients and our staff. But in order to harness the full potential of these whole room systems, you should start with a thorough assessment of your infection prevention needs and a collection of perspectives from across your team.
If you are considering making the plunge into whole room technology, here’s a primer on the latest options and the key questions you should consider to meet your facility’s needs.
UV as a core strategy
UV radiation — also called UV germicidal irradiation (UVGI) — became much more commonplace during the pandemic as a core strategy to augment manual cleaning.
These no-touch technologies help eliminate microorganisms within the environment. UV systems are usually pretty straightforward to operate, whether you opt for a disinfecting robot that’s placed in a room or a system that’s strategically positioned to hit all the exposed surfaces in your OR.
Before purchasing a UV system, assess your environmental staff’s comfort with new technology, their existing workflows and the overall needs within your facility. The type of UV system you choose — and the number of units you need — will depend on the size of your facility and the bandwidth of your team to bring new equipment into their infection control workflow. Know that this technology won’t ever replace the manual cleaning that must happen in between procedures or at the end of the day, but it can offer an enhanced layer of additional disinfection protection to your repertoire.
Consider the layout of your facility and if the UV light will reach all exposed surfaces. It’s also important to note that the light range will vary from unit to unit. You want to make sure your UV system is close enough to all the exposed surfaces to maximize the benefits of this tech.
Once you’ve completed the analysis of your space and trained your staff, UV robots are fairly easy to operate: You put it in the room, close the door and let it go. For safety, these systems usually have occupancy sensors and remote starters to ensure staff have exited before they get to work.
Misters and visible light systems
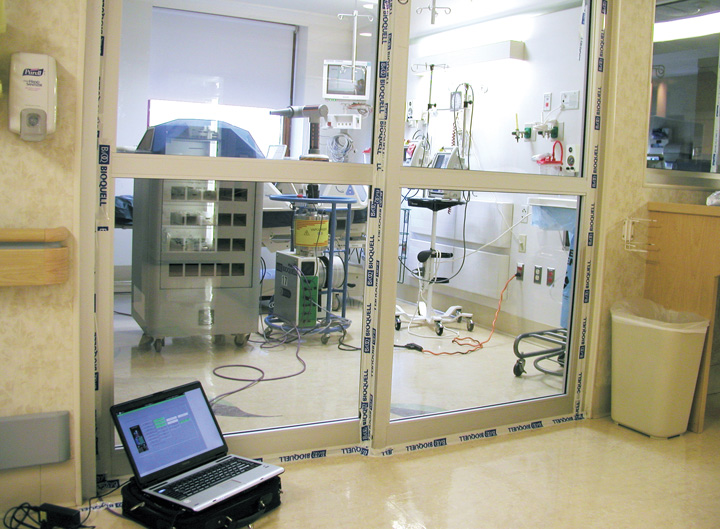
Beyond UV, hydrogen peroxide mister systems offer another option to bolster disinfection and infection prevention. These systems use aerosolized, or fogged, hydrogen peroxide to clean the surrounding environment, helping to eliminate bacterial, fungal and other microbial threats that may linger on surfaces or in other hard-to-reach areas. Remember, you need to account for every threat you can before you have a larger problem.
With all chemical disinfectant systems, take inventory of the equipment in the room. The last thing you want to do is spray a chemical mist in your OR that puts your seven-figure surgical robot out of commission. Be sure that your surgical equipment and your chemical disinfectants are compatible.
Secondly, it’s important to understand these systems all come with unique defined terms of use, and compliance is key to ensure you’re getting the full benefit. All chemical disinfectants have a dwell time that the product must remain on surfaces to kill pathogens. You’ll need to build this time into your overall workflow. Like UV, these systems require trained staff to operate them. They typically require your team to don full personal protective equipment (PPE) during application to avoid exposure. Your entire staff needs to be cognizant of when your misters are in effect to avoid exposure. Put procedures in place to ensure your team knows when they can safely re-enter the room. The legwork with these systems starts on the front end, and you will want to evaluate how a chemical disinfectant fits within your existing cleaning process.
While UV and hydrogen peroxide are the most common whole room systems on the market, there are other options such as visible-light continuous environmental disinfection (CED) systems — tech that uses visible light to offer automatic, non-stop disinfection — that are gaining traction, particularly in the hospital sector. While I don’t have any direct experience with the technology, it doesn’t mean CED isn’t a viable option. For instance, there’s research showing these systems help reduce bacterial surface contamination.

Maximizing your whole room disinfection system begins with conversations across your organization to assess your needs. To that end, here are a few key questions to ask your team.
- How are you conducting postoperative surveillance? Do you have a way to assess environmental transmission of MRSA, C. diff or other organisms?
- What does your cleaning/disinfecting process look like, and how would this new technology impact turnaround times?
- What is the capacity of your staff to train and implement new technology?
- What is the evidence-based science to justify a new system?
- What facility-specific questions do you need to answer to evaluate the benefits of whole room disinfection?
Staying on top of the latest technology ensures you are doing everything you can to protect your staff and your patients. Attending conferences and conversations with vendors are great starting points to identify the platforms that may work best for your facility. You’ll want to balance the upfront and ongoing costs against the potential benefits that supplemental cleaning can bring to your facility to prevent the spread of harmful pathogens.
—Benjamin D. Galvan, MLS(ASCP), CIC, CPH
Multidisciplinary insights
When it comes to bringing any new disinfection technology into your facility, you should keep the big picture in mind. That means considering viewpoints from across your team.
Even if you don’t have a dedicated infection preventionist on staff, you need continuous surveillance in place to capture your weak points. Monitoring surgical site infection rates and postoperative follow-up with surgeons can help reveal problems with your disinfection and cleaning. You want to identify these trends before they lead to larger problems for your facility and your patients.
Secondly, consult with your staff members on the front line. These individuals have the best understanding of what can be done within their overall workflow and how to safely and efficiently implement new technology. Whole room systems work best when you follow the instructions, but we know there will always be human factors at play. For instance: Your chemical disinfectant might work great, but if it has a foul smell, you’re almost guaranteed to have issues getting staff to use it properly. Getting feedback early on can improve and streamline the implementation of any new technology.
Facility managers will also have important insights about staffing. We’re all well-versed on staffing shortages in health care. Evaluate how supplemental cleaning technology may help your staff as they handle their disinfection duties alongside other new responsibilities they may have. Improving your disinfection processes can offset the risks that have always existed, particularly in high-risk settings like orthopedics and other highly invasive procedures.
Finally, you’ll want to check in with your materials management and procurement teams to understand how this technology fits into your facility. If you add a new system to your cleaning process, make sure you have a secure supply chain you can count on. For instance, if you’re using a hydrogen peroxide whole room product, ensure you have the PPE available in sufficient supply for staff as well as sufficient disinfectant product, etc.
A true cost-benefit analysis
Being fiscally responsible is a core part of infection prevention. It’s impossible to eliminate every risk, but we must regularly evaluate the ways we can improve our processes. We also should come to the table with realistic expectations about how much our facilities can afford to invest in new platforms. A strong cost-benefit analysis will help you weigh the pros and cons of any new technology. Consider the costs of new technology against the potential benefits to prevent healthcare-associated infections (HAIs). If your facility is seeing environmental transmissions for MRSA, C. diff or other organisms, it’s worth your time to consider bolstering your processes and your supplemental cleaning options.
Your cost analysis should factor in the acquisition of new technology, the time and labor it takes to train staff on it, and any related materials you may need to purchase on an ongoing basis. Like all major purchasing decisions, you’ll want to review the latest clinical evidence and research to justify any whole room technology you bring on. The true cost of HAIs is difficult to estimate, but it’s in the billions nationally each year when you account for added length of stay, follow-up care, loss of productivity and diminished quality of life.
Prioritizing infection prevention helps limit some of the continuous risks we face working in health care, and it’s an integral part of every successful surgical facility. The pandemic taught us we all must strive to stave off the infectious pathogens that are lurking just around the corner. While whole room disinfection technologies aren’t quite the standard of care in most ORs just yet, there’s no doubt they offer a strong potential option to augment your infection prevention efforts. OSM
.svg?sfvrsn=be606e78_3)
.svg?sfvrsn=56b2f850_5)