• Tailor the treatments. Multimodal prevention strategies ensure that patients at risk of PONV receive optimal prophylaxis measures. Effective and appropriate therapies should be based on a patient’s risk factors, health history,
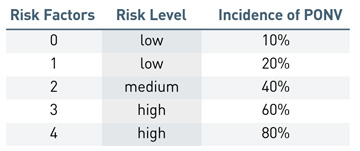
input from the patient and the cost-effectiveness of the treatment. Use PONV risk scores to guide the care of individual patients. The Apfel risk score is based on four factors: female sex, history of PONV/motion sickness, non-smoking status
and use of opioids after surgery.
Base your decision on when to administer preventative treatments by determining how many risk factors are present during a given case. The latest PONV consensus guidelines recommend the use of multimodal
prophylaxis in patients with one or more risk factors.
Start by administering dexamethasone (a corticosteroid) after induction of anesthesia and ondansetron (a 5-HT3 receptor antagonist) five to 10 minutes before emergence at the end of the case. Both drugs have proven to be effective in preventing
PONV when used in combination. Patients with three or more risk factors generally require a more aggressive multimodal approach involving the avoidance of inhalational anesthetics and the use of total intravenous anesthesia (TIVA), with propofol
induction, minimal or opioid-free pain management and preferential use of regional anesthesia as part of a multimodal approach for enhanced recovery pathways.
Propofol TIVA completely eliminates the use of inhalational anesthetics such as sevoflurane, isoflurane and desflurane, which are emetogenic by nature. When used in combination with other prophylactic agents, propofol TIVA further reduces the
risk of PONV. Administering epidurals and local blocks to minimize the reliance on opioids such as fentanyl, morphine and hydromorphone — which are also emetogenic — and to manage post-op pain is key to preventing PONV in high-risk
patients. IV acetaminophen has been shown to reduce nausea when used as part of a multimodal analgesic strategy and administered before the onset of pain.
• Minimize fasting. Ensuring patients remain adequately hydrated by limiting pre-op fasting or administering supplemental intravenous fluids during surgery is an important element of an effective preventative strategy. There has been
a complete shift in the past five to 10 years regarding fasting before surgery. Patients are now generally encouraged to drink clear, carbohydrate-rich drinks up to two hours before their surgeries.
Research has shown preoperative carbohydrate loading keeps the body’s insulin response at a steadier level than fasting for extended periods before surgery. Patients who have been fasting can be extremely hypotensive after anesthesia induction.
Hypotension and dehydration have been linked to increased risk of PONV.
• Try adjunct remedies. Although there is a lack of robust clinical evidence supporting the efficacy of alternative therapies in the prevention of PONV, incorporating non-pharmacological treatments into multimodal prevention strategies
provides some benefit. For example, using acupressure to stimulate the pressure point PC6, which is located on the inner wrist, has been shown to significantly reduce nausea and vomiting. Aromatherapy helps to reduce the need for rescue antiemetics
for patients who feel ill in recovery. Higher doses of oral ginger (1,000 mg) can cause a small reduction in nausea scores and contribute to better outcomes. Preliminary research also shows that chewing gum is as effective as ondansetron in
preventing PONV in women who undergo laparoscopic breast surgery under general anesthesia. Even music therapy has shown some evidence of reducing the risk of PONV.
• Be ready to rescue. When prophylaxis measures don’t work and patients feel sick in recovery, administer an antiemetic medication from a different class than what they received during surgery. Repeating the same dose of the
same agent within six hours of the last administration will not inhibit PONV, and therefore fail to provide therapeutic benefits. Amisulpride (a D2/3 antagonist) is a recently FDA approved drug that can be used as a rescue medication for patients
who are experiencing PONV after failed prophylaxis. Other products that can be used include NK-1 receptor antagonists, antihistamines and anticholinergics.
.svg?sfvrsn=be606e78_3)

.svg?sfvrsn=56b2f850_5)