The latest devices and techniques help surgeons reduce SSIs by better managing incisions.
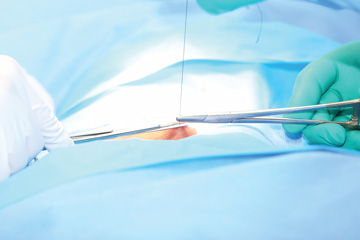 FINAL STEP Layered closures with absorbable suture help to prevent infections after open procedures.
FINAL STEP Layered closures with absorbable suture help to prevent infections after open procedures.
Nothing is more devastating than a preventable surgical site infection (SSI) complicating an otherwise perfectly executed procedure, which is why effective management of a surgical wound is as important as the surgery itself. Wound care should be a top priority, not an afterthought. Thankfully, multiple advances in closure devices and closing techniques are helping OR teams keep their infection rates low while helping patients recover more quickly.
The three tenets. Safe and efficient wound care based on tight closures, adequate blood flow and sterile dressings are the keys, according to J. Gabriel Horneff III, MD, FAAOS, an assistant professor of clinical orthopedic surgery in the shoulder and elbow division at Penn Medicine in Philadelphia. "For open surgeries, I recommend a thorough washout using approximately three liters of irrigant," says Dr. Horneff. "If the case involves treating a previous infection, use a total of six to nine liters. I primarily use sterile saline mixed with tobramycin or another triple antibiotic, which can be administered in multiple ways."
Pulse irrigation, which works particularly well for orthopedic cases, involves a battery-powered gun that shoots the irrigation mixture into the wound in jet spurts, says Dr. Horneff. "This method irrigates the wound and achieves a good mechanical debridement that is needed in cases involving concerns about a wound's healing capabilities," he says.
Closures and dressings. Dr. Horneff believes layered closures are the best way to prevent surgical wound infections in open surgeries. "Vicryl sutures for the deeper fascial and subcutaneous layers are best, followed by Monocryl suture for the skin layer," he says. "Both options are absorbable, but Vicryl suture is braided and lasts a little longer than Monocryl suture, which is made of monofilament. After placing the suture, surgeons should bury the knots in the tissue."
Vacuum suction dressings. Negative pressure therapeutic wound-care devices have improved significantly over the last 10 years and have impacted core ideas on wound healing. These battery-powered devices, no bigger than a purse, keep wounds sterile while using negative pressure to suck fluids from the wound and enhance blood flow to the area. Surgeons place a vacuum sponge atop closed incisions, and patients can remove the tube that connects the dressing and the device when they take a shower and reattach it afterward.
"The most important thing when caring for a fresh wound is minimizing what the patient must do to manage it," says Dr. Horneff. "Any solution that eliminates the patient's need to remove dressings or make sure their stitches aren't protruding from the skin is a good thing."
That's where absorbable sutures, waterproof dressings and other products and devices come in. They eliminate potential sources of aggravation during recoveries by allowing surgeons to close off incisions from the environment, ensure healthy blood flow to the wound and keep everything covered and sterile. "All of that is best performed by providers, not patients," says Dr. Horneff.
.svg?sfvrsn=be606e78_3)



.svg?sfvrsn=56b2f850_5)