Dr. Shorstein points to several studies that show cataract patients — in the case of one highly regarded study, 93% of them — instill drops incorrectly. They touch the tip of the eye drop bottle, scrape the cornea during administration
or miss the eye altogether. “That’s worrisome because it’s important that patients receive the drops without traumatizing the eye to prevent post-op infection and inflammation,” he says.
Dropless cataract surgery eliminates these concerns. There are several options available to perform it while making life simpler for patients.
• Intracameral injections. At the end of standard procedures, Dr. Shorstein injects the antibiotic moxifloxacin into the eye’s anterior chamber. “It’s extremely effective in reducing the risk of endophthalmitis,”
he says. “Our rate is about one in 5,000 patients.”
There still is no FDA approved moxifloxacin product indicated for this use, so the drug must be compounded by a 503B outsourcing pharmacy. It’s essential to source moxifloxacin from a vetted facility. “Ordering it, setting up shipping
and having it stored properly — that takes some preparation and time,” says Dr. Shorstein.
Practice changes evolve over time, and I think dropless surgery is where we’re heading.
— Neal Shorstein, MD
When European surgeons began administering intracameral injections of antibiotics two decades ago, they initially also prescribed topical drops. “The thought was, ‘I’ll just add the injection to what I’m already doing,
and we’ll make absolutely sure that we’re going to prevent infections,” says Dr. Shorstein.
Swedish researchers then produced several studies in the late 2000s and the 2010s that found 85% to 90% of surgeons in that country had evolved to injection-only cataract surgery. (In Europe’s case, intracameral cefuroxime is typically
used instead of moxifloxacin.)
“Instilling topical antibiotic drops has been the traditional practice for surgeons, even though prior to 2016 no research showed that drops reduce the risk of endophthalmitis,” says Dr. Shorstein. “But more recent studies
say topical drops reduce the load of bacteria on the eyelid and even on the conjunctiva.”
Many surgeons in the U.S. still prescribe topical antibiotic drops in addition to administering the intraoperative injection. Dr. Shorstein suspects that’s due to habits prevailing for decades, but emerging research continues to favor
the dropless trend and increasing numbers of physicians are realizing topical drops aren’t necessary when injections are administered. “Practice changes evolve over time, and I think dropless surgery is where we’re heading,”
he says.
At the end of surgery, Dr. Shorstein also injects triamcinolone, a long-acting steroid, into the subconjunctival space to prevent post-op inflammation. He says the injection — an off-label use of an FDA approved product — is as
effective as administering topical steroid drops.
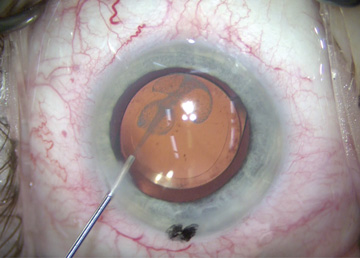
• Sustained-release meds. Two FDA approved products have recently emerged to give surgeons another effective option for administering the steroid treatment. Dexycu (dexamethasone intraocular suspension) 9% is a steroid injected
behind the iris in the inferior portion of the posterior chamber. Dextenza (dexamethasone ophthalmic insert) 0.4 mg is inserted into the punctum.
“Both of these products remain in place for about two to three weeks and provide long-acting steroid administration to the eye,” says Dr. Shorstein. “By administering these agents, surgeons take control of ensuring the drugs
are in place for prophylaxis. It definitely gives us peace of mind, and patients love the practice because they don’t need to constantly put in drops throughout the day.”
Dr. Shorstein acknowledges the two medications are expensive, ranging in price between $500 and $700 per case. However, both agents have received pass-through status from CMS, meaning facilities can bill CMS separately for their use and be
reimbursed the average sales price plus 6%. Dexycu has pass-through status through March 31 of next year and Dextenza’s pass-through status is set to expire at the end of December. However, CMS has indicated in its proposed 2022
Hospital Outpatient Prospective Payment System — the final rule is expected to be published this month — that it will extend the pass-through status for both medications until the end of next year.
Surgeons might soon have another way to perform dropless cataract surgery. The concept of soaking IOLs in an antibiotic and non-steroidal solution prior to implantation is currently being studied, according to Dr. Shorstein, who’s excited
by the possibility. “If you supplement a soaked implant with an intracameral antibiotic injection, the amount of antibiotic drug present in the eye is very high initially and persists for numerous days after the surgery,” he
says. “This is a very exciting area, and if it comes to market, it has the potential to be a complete gamechanger.”
.svg?sfvrsn=be606e78_3)
.svg?sfvrsn=56b2f850_5)