Ms. Ulmer's initial lobbying for surgical smoke safety began in the 1990s on the national level. She spent significant time in Washington working on language with OSHA representatives for a bill that would have required the evacuation of
surgical smoke in ORs across the country. The legislation was introduced, but ultimately died in Congress. Two decades later, a national ban on surgical smoke is no closer to becoming reality. The good news, says Ms. Ulmer, is that local legislation
can be just as effective.
"Nurses and technicians have grown tired of nothing happening, which is why you're seeing so much activity at the state level," she says.
Smoke safety is a personal issue for Ms. Ulmer as well. After she joined AORN's board in the 1990s, she'd work in the OR only once per month. "After one day of high-smoke-producing cases, my nose burned, my throat hurt, my chest was tight and
I felt nauseous," says Ms. Ulmer.
She felt fine the next day, but experienced the same symptoms a month later after a full day spent in the OR. "I made the connection that when I'm away from the smoke, my body starts to feel normal again," says Ms. Ulmer. "I decided then that
surgical smoke was really bad for your health, and that's what started me on this journey."
When Ms. Ulmer stopped working in ORs full-time in 2012, her primary care doctor said she had a "90-day cough," and an allergist diagnosed her with adult-onset asthma. "I had a lot of respiratory issues," she says.
Ms. Ulmer knew her story wasn't unique, as the unusually high rate of perioperative nurses with respiratory illnesses had been well-documented. Her own health history, the reported problems of fellow nurses and smoke evacuation legislation passed
in Rhode Island and Colorado inspired Ms. Ulmer to begin working toward getting a similar law passed in Georgia. After proposing the initiative to Georgia Council Chair Pat Thornton in 2019, she was asked to chair the council's legislative
committee. She and a small core group started contacting local legislators to seek support for smoke legislation. Their persistent efforts eventually resulted in gaining the support of Senator Gloria Butler. However, it would take a serendipitous
encounter to make it happen.
Senator Butler's annual fish fry was scheduled to take place in October 2019, and Ms. Ulmer made it a point to attend. She had been calling the senator's office so often to discuss smoke evacuation legislation that her staff knew her by
name. Still, her calls went unreturned.
At the fish fry, Ms. Ulmer walked right up to Senator Butler. "I held out my hand and said, 'I'm Brenda Ulmer,' and she said, 'I know about you!' So she had gotten my messages!"
Ms. Ulmer gave Senator Butler materials from AORN about smoke evacuation, which she held in her hand as she addressed the crowd. After the fish fry, though, Ms. Ulmer didn't hear from the senator, so she and the legislative committee continued
contacting and meeting with other legislators in the Georgia Senate and House. The legislative committee traveled to AORN chapters around the state to talk about smoke and build a statewide coalition, which they called the Smoke Busters.
On New Year's Eve 2019, Ms. Ulmer's phone rang at 10 p.m. It was Senator Butler calling to say she would sponsor a smoke evacuation bill. Ms. Ulmer hung up the phone, stunned by the senator's out-of-the-blue support. With Senator Butler now on
board, the Georgia Smoke Busters were about to get a crash course in lobbying and lawmaking.
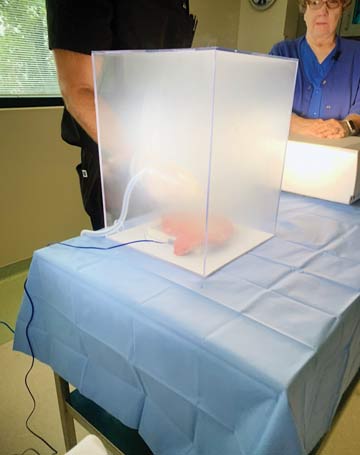
A few months later, a smoke evacuation bill began to take shape in the Georgia General Assembly. A hearing was held, but then the pandemic shut down the legislature. When lawmakers reconvened in the summer, Senator Butler introduced and helped
pass a resolution that required the Senate to convene a smoke study committee, which held meetings each month in the fall. Senator Butler included Ms. Ulmer and the legislative committee in developing the agendas aimed at educating the legislators
on the hazards of surgical smoke.
Ms. Ulmer says she was working 30 to 40 hours a week on the legislation effort throughout 2020. She and legislative committee members traveled to AORN chapters around the state to drum up support and encourage perioperative nurses to contact their
local legislators. It was during that massive networking effort that Ms. Hohn's story came to light.
Jennifer Pennock, AORN's senior director of government affairs, was working with the Georgia team on their lobbying efforts. She asked Ms. Hohn to testify before the senate committee by writing a letter that could be read to its members. "I wrote
what I thought was my first draft, and video-called with the smoke evacuation team to read it," says Ms. Hohn. "Afterward, everybody was silent. Then one person finally said, 'You're incredibly brave. Don't change anything. We want you to
be the first presenter to the committee because your message is so powerful.'"
.svg?sfvrsn=be606e78_3)


.svg?sfvrsn=56b2f850_5)