Retained foreign objects were the most frequently reported adverse event between 2015 and 2017, according to The Joint Commission. We decided to tackle this issue head on by developing a custom count board at our surgery center that could be used in all of our health system's outpatient facilities. Here are the key elements that make it an effective way to keep track of every sponge, needle, burr and blade used during surgery.
- Frontline feedback. A number of perioperative nurses and certified surgical technologists came together to modify our health system's inpatient count worksheet into a custom dry erase board that now hangs in each OR. Staff members who came to our ASC from inpatient units were accustomed to using the standardized count worksheet, but colleagues coming from other outpatient facilities within the health system were already familiar with using a whiteboard to display counts. The group liked the worksheet's format, but wanted the counts visible on an easy-to-reference whiteboard.
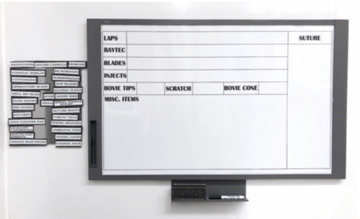
- Intuitive design. We combined our internal policy for preventing retained surgical items with AORN guidance to develop a whiteboard used to track soft goods, sharps and miscellaneous items. The count board's design needed to follow the established sequence in which the counts should be conducted (sponges, sharps and miscellaneous items) using the standardized count worksheet as a guide. The staff split into groups to create their ideal board. For example, one group came up with the idea to put the column for sutures on the far right so that additional suture added to the field could be counted vertically instead of trying to add numbers together horizontally. The groups then came together and designed a board taking into consideration all ideas presented.
.svg?sfvrsn=be606e78_3)
.svg?sfvrsn=56b2f850_5)