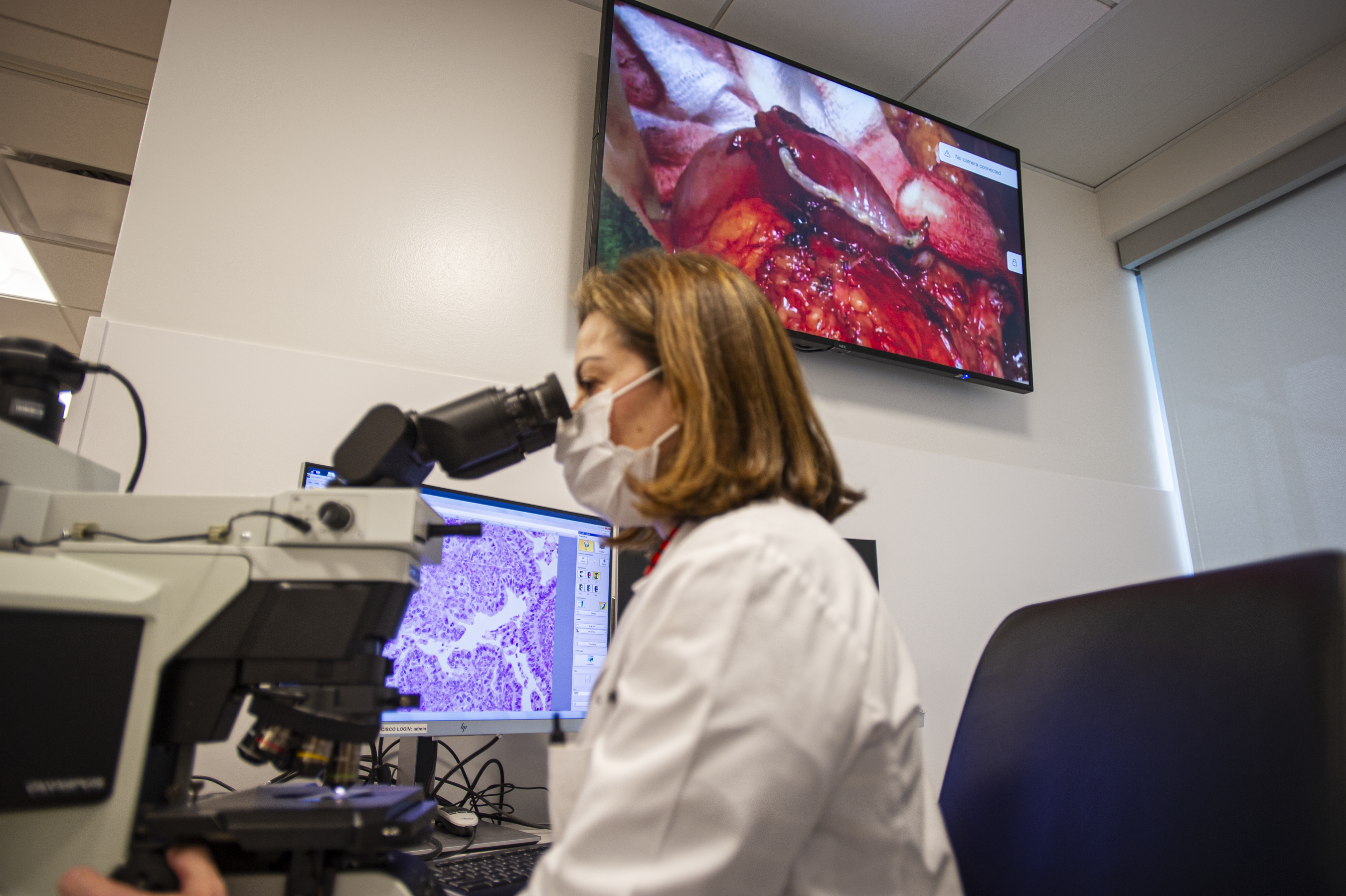
Both Ms. Chua and Ms. Milam rave about the ability their video integration systems provide for increased collaboration not only inside the OR, but beyond the walls as well. Videoconferencing in particular is a major benefit. Take, for example,
an intraoperative biopsy. Previously, says Ms. Chua, the surgeon would remove tissue and send it to pathology for dissection. Then the pathologist would walk to the OR or use the phone to tell the surgeon if the sample was sufficient or if
more tissue was needed. Now, thanks to cameras embedded in the OR's surgical lights, the surgeon can simply share image of the surgical field, live, with the pathologist sitting in their lab or office. "The two of them can have a conversation
through the speakers in the OR about whether to finish the procedure or continue removing tissue," she says.
At Ms. Milam's facility, surgeons in different ORs can consult while performing surgeries. "For example, a GYN surgeon working in one OR and a general surgeon working in another can share video images in real time on each other's screens and discuss
what they see," she says. Her facility has used video integration to show live surgeries in its conference rooms for teaching purposes, too.
In a video integration system, all images and videos are managed and processed through what is essentially a combined server and router. This enables videoconferencing and can deliver those images and videos to EMRs.
This capability has made a big difference at Ms. Chua's facility. Previously, patient info was manually entered to tag images and videos from surgeries, and staff had to print numerous copies of images to add to medical records for the surgeon
to evaluate and to share with patients and their caregivers. Now all OR staff need to do is open the patient's EMR.
"From there, it automatically interfaces the video system," says Ms. Chua. "When the surgery is complete and the surgeon is informing the patient's family, they've already pulled all the pictures and annotated them. If they have 20 pictures and
only want to give the patient three that reflect the procedure, they just add those images into their discharge notes."
Perioperative professionals must be well-versed in the capabilities and operation of video integration before they use it in live procedures. At Ms. Chua's facility, an in-service was held with a large group, followed by one-on-one trainings for
each staff member. She says her tech-savvy staff was off on their own within a week. But it's not just the surgeons and OR staff who need to be comfortable with the new equipment and technology. "We also wanted to make sure our ancillary team
and support services were comfortable, because they're the ones who need to do the preparation, upkeep and end-of-day cleaning of the area," she says.
Ultimately, video integration is way more than pretty pictures. It allows surgeons, OR and support staff to work more quickly, intelligently, precisely and collaboratively. OSM
.svg?sfvrsn=be606e78_3)


.svg?sfvrsn=56b2f850_5)