Obstructive sleep apnea (OSA) is a common disorder affecting approximately one in four adults. It's also often undiagnosed — 90% of people with OSA don't know they have it — and undertreated. Failure to appropriately assess patients for the disorder increases the risk of complications during and after surgery, including prolonged recovery and, worse, adverse respiratory events.
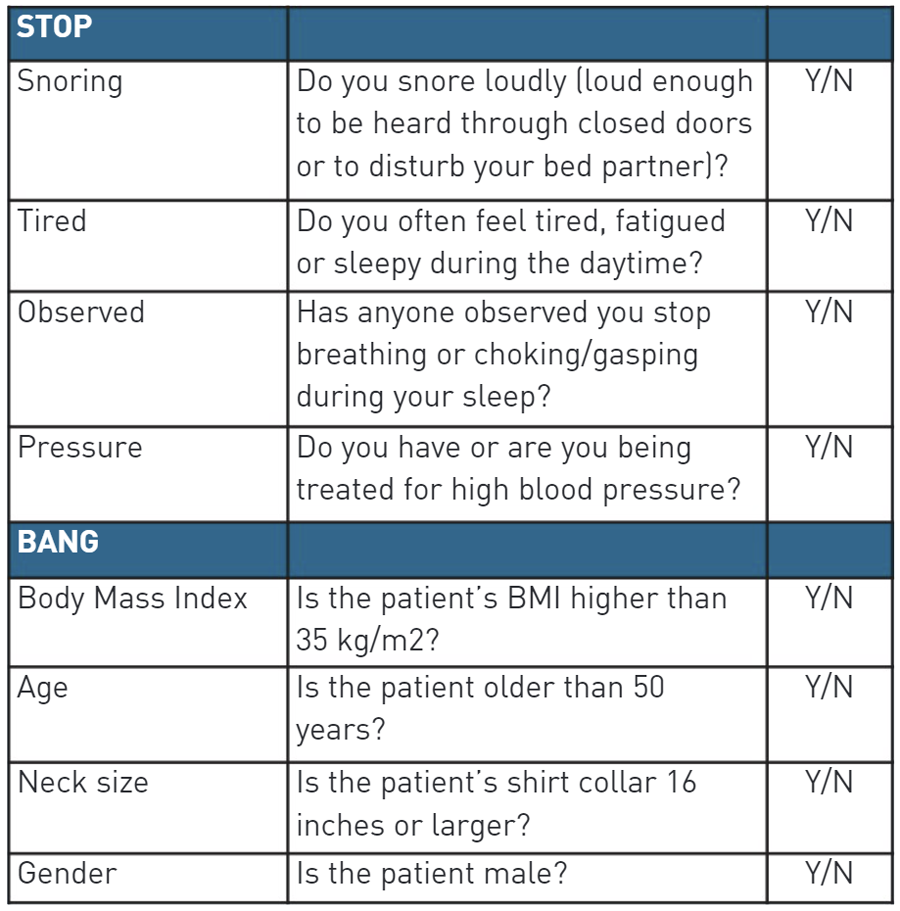
We had been using the STOP — Snoring, Tiredness, Observed Apnea and Pressure (hypertension) — tool to assess patients for OSA before they underwent endoscopy cases. One patient who we identified as having OSA was still heavily sedated after a procedure. Over-sedation can lead to respiratory depression or compromise and the patient's condition can quickly deteriorate. That caused us to take a second look at the protocols we had in place to assess patients for OSA as well as the steps we take to keep them safe.
After some research, we realized the STOP tool collects only subjective data. For example, many patients aren't aware they snore when they're asleep. By adding "Bang" (BMI, Age, Neck Circumference and Gender) to the questionnaire, we were able to identify more patients who presented with OSA. When a patient is appropriately screened for OSA and exhibits signs of complication risks, providers can implement interventions that lead to safer procedures.
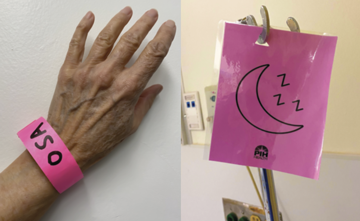
- Highlighting at-risk patients. When we perform the initial screening for OSA using the STOP-Bang questionnaire and the patient identifies as high-risk, we place a bright pink band on their wrist and hang a pink sign on their bed. This alerts providers that they need to put appropriate precautions in place.
- Involving anesthesia. Sedation for upper endoscopies is tricky because the patient is typically placed in the lateral, semi-prone or prone position, which greatly reduces the anesthesia provider's access to the airway. High-risk OSA patients undergoing upper-endoscopy procedures are well-suited for monitored anesthesia care (MAC) administered by anesthesia providers who are experts at airway management. Anesthesia providers also administer MAC with propofol, which is a short-acting sedative that reduces the risk of over-sedation.
During the procedure, anesthesia providers use a multi-port capnography mask, which allows for preoxygenation of the patient and easy access to the nose and mouth. It also has a capnography sampling port for continuous monitoring of the patient's end-tidal CO2. Anesthesia providers are prepared to employ the head-tilt-jaw-lift technique and ensure adjunct airways are readily available in the event the patient's airway becomes obstructed.
- Remaining vigilant in recovery. After procedures, OSA patients are placed in a lateral or semi-upright position — if the positions are not contraindicated — to help open up the airway. It's important for the PACU staff to monitor patients closely for any complications and to have airway management equipment nearby. Before patients are discharged, reinforce the importance of managing and treating OSA, and advise them to follow up with their primary care physician for further evaluation.
.svg?sfvrsn=be606e78_3)
.svg?sfvrsn=56b2f850_5)