Four ways your care team can combat SSIs.
 Covering sterile tables can reduce bacterial contaminations at four and eight hours, according to a study published in American Journal of Infection Control.
Covering sterile tables can reduce bacterial contaminations at four and eight hours, according to a study published in American Journal of Infection Control.
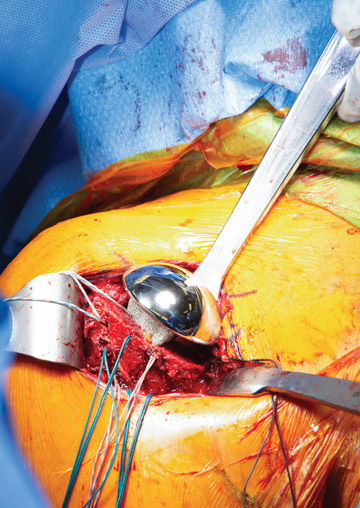
Surgical site infections (SSIs) are always top of mind for any OR team as they implement procedures and employ strategies for patient safety. Whether you’re doing total joint procedures today or plan to add them in the future, it’s important for your staff to have the tools and knowledge available to them to help prevent, diagnose and treat surgical site infections.
SSIs are expected to increase by an alarming 198% by 2023 for knee and hip replacements, and the cost to the healthcare system for knee and shoulder infections is projected to reach $1.62 billion.1 Today, surgical site infections contribute to the most common reasons that knee and hip surgeries require a second visit to the OR for revisions.2
Clearly, a focus on SSIs and ways to reduce them is of critical importance in total joint procedures and it's equally critical that your staff is armed with the best resources to help reduce SSIs. Here are four ways to help reduce SSIs.
Begin with the skin. About 80% of skin flora occurs on the outer skin layers.2 In fact, one square centimeter of skin can host as many as 10 million aerobic bacteria, a leading cause of healthcare-acquired infections.1 A single-use skin prep applicator can help reduce skin flora by moving the clinician’s hand away from the patient’s skin for a more aseptic technique (this does not apply to the swabstick format). A proprietary tinting process also allows the clinician to see the prepped area more clearly.
Tables take cover. Are you covering your tables and stands? The Association of periOperative Registered Nurses (AORN) guidelines state that the sterile field – including tables – should be covered if not being used immediately.3 You can help significantly reduce the risk for contamination by covering even just portions of the sterile field that are not in active use.3
The American Journal of Infection Control recently published a study stating that covering sterile tables reduced bacterial contaminations at four and eight hours. The study also suggested that covered tables reduce the amount of bioburden that can collect on unused instruments.4
Beware the colonies. Research suggests that the risk of SSI increases up to nine times due to nasal colonization of Staphylococcus aureus, presenting a big challenge in surgical settings.5 Pre-op testing for MRSA is not always included at surgical facilities, but some proactive clinicians have modified their pre-op protocol to treat every surgical patient with a nasal iodine-saturated swab, often with favorable results.6 Nasal swab tests allow clinicians to detect and identify MRSA for better prevention and control. Scalable instrument models fit into a wide variety of testing environments, including surgery centers that are usually challenged for space.
Dress for success. Not all orthopedic surgical gowns are created equal. High-quality surgical gowns should meet or exceed testing standards of the American National Standards Institute and the Association for the Advancement of Medical Instrumentation, and they should be certified to meet AAMI level 3 standards for all critical zones. When selecting a gown, be sure to choose one that’s resistant to tears, punctures, strikethrough and fiber strains — and also is comfortable for your staff to use every day.
Note: For more information on SSI prevention and products that help reduce infections in total joints, please go to visit the McKesson orthopedics webpage.
References:
1. Kurtz SM, Lau E,Watson H, Schmier JK, Parvizi J. Economic burden of periprosthetic joint infection in the United States. J Arthroplasty. 2012; 27(8) (suppl):61-5.e1.
2. Readmission Rates, Causes, and Costs Following Total Joint Arthroplasty in US Medicare Population, W. Murphy, P. Lane, B. Lin, T. Cheng, D. Terry, S. Murphy; Bozic KJ, Kurtz SM, Lau E, et al. The epidemiology of revision total knee arthroplasty in the United States. Clin Orthop Relat Res. 2010; 468(1):45-51.
3. AORN Guidelines for Perioperative Practice, 2018 Edition
4. Markel, et al. Covering the instrument table decreases bioburden: An evaluation of environmental quality indicators, American Journal of Infection Control, 2018
5. Price CS, Williams A, Philips G, Dayton M, Smith W, Morgan S. Staphylococcus aureus nasal colonization in preoperative orthopaedic outpatients. Clin Orthop Relat Res. 2008; 466(11):2842-2847.
6. Outpatient Surgery Magazine, 2018
7. Melissa S. Schmidt, MSN, RN, CNL, CPAN, CAPA, PACU.; VandenBergh MF, Yzerman EP, van Belkum A, Boelens HA, Sijmons M, Verbrugh HA. Follow-up of Staphylococcus aureus nasal carriage after 8 years: redefining the persistent carrier state. J Clin Microbiol.1999; 37:3133-3140.
 HEALTHY START Optimizing the nutritional status of patients leading up to surgery can be part of a multifaceted infection prevention strategy.
HEALTHY START Optimizing the nutritional status of patients leading up to surgery can be part of a multifaceted infection prevention strategy.
.svg?sfvrsn=be606e78_3)


.svg?sfvrsn=56b2f850_5)