The effort demanded determination, hard work and passionate selling of the health-related benefits.
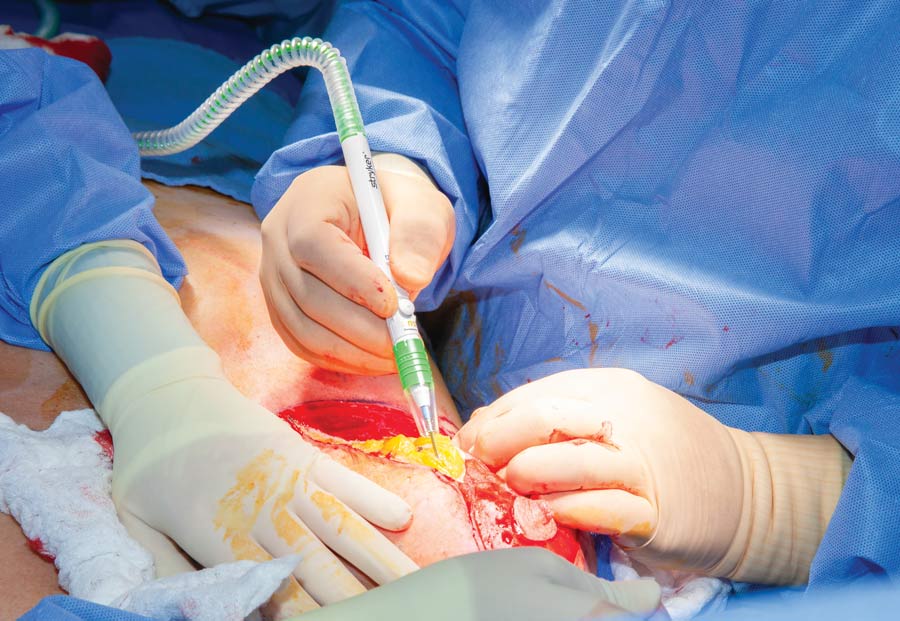
 CREDIT: MedCenter Mebane Surgery Center
CREDIT: MedCenter Mebane Surgery CenterFRESH AIR Tabitha Turner, RN, MSN, CNOR, CGRN, educates staff on the dangers of surgical smoke.
The dangers of inhaling surgical smoke seem obvious, but affecting change at a facility to ensure smoke evacuators are installed and used is much less straightforward. Tabitha Turner, RN, MSN, CNOR, CGRN, assistant director at the Cone Health MedCenter Mebane (N.C.) Surgery Center, and the driving force behind its implementation of a surgical smoke evacuation program, understands that quandary very well.
After attending a medical conference where she learned about the Association of periOperative Register Nurses' (AORN) Go Clear program, Ms. Turner dove deeply into the issue, spending two months on research she presented to her leadership, which voiced its support. She then collected every study and article she could find about surgical smoke and bound it into a book she passed out to staff and surgeons. Each week, she posted new information about smoke evacuation on bulletin boards throughout the center. She placed packets of research in locker rooms and lounges, and even gave the surgical team candy cigarettes to get across the point that surgical smoke, like cigarette smoke, is dangerous to your health.
It didn't take long to convince staff and surgeons to join the smoke-free movement. "I spent many months gathering data to support what I was talking about," says Ms. Turner. "It's really important to present surgeons with clinical evidence when asking them to change how they operate."
In just over a year, Ms. Turner established a smoke evacuation program. She walked away with these valuable lessons:
- Show the newest models. Ms. Turner brought in sales reps to introduce the latest smoke evacuators and set up trials. When her health system's ENT surgeons expressed concern about the potential negative impact of a smoke evacuation pencil close to the surgical site, she worked closely with them to gain their support. She then proceeded to win over the orthopedic and general surgeons. Much of the opposition came from experiences surgeons and staff had with earlier smoke evacuation products, so the design and functional improvements in the new devices, such as slimmer profiles, incorporation into electrosurgery devices and quieter operation, bolstered her case.
- Choose the correct filters. After staff and surgeons began to use smoke evacuators during procedures, Ms. Turner continued educational efforts to ensure the devices were being used properly. She discovered many facilities don't use the correct filters, so she referred to the evacuators' instructions for use and ensured surgical teams understood the importance of using the correct filters.
- Wear proper PPE. For added protection, ASTM level 3 masks should be used during smoke-producing cases. Higher-grade surgical laser masks should be used for procedures expected to generate heavy amounts of plume.
Ms. Turner has expanded her smoke evacuation program to facilities throughout the Cone Health system. With mandatory smoke evacuation laws now in place in three states, with more potentially on the way, Ms. Turner says the time for facilities to act is now. "It's going to be managed for you at some point, so get ahead of it," she says. "Pick out the products you want and make your own path. Don't wait for somebody to tell you what to do."
.svg?sfvrsn=be606e78_3)


.svg?sfvrsn=56b2f850_5)