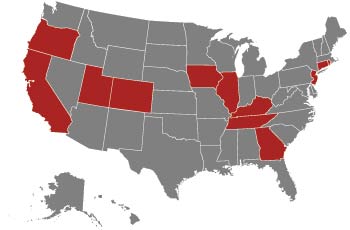
AORN, state associations and individuals have been working steadfastly with state legislatures around the country to ensure the use of smoke evacuation systems in ORs. It's been a long slog, but the massive effort is paying dividends. Here's a
snapshot of the current status of legislation around the country, as provided by AORN Senior Director of Government Affairs Jennifer Pennock.
Ms. Pennock says the COVID-19 crisis impacted AORN's surgical smoke legislative efforts this year. "Across the country, state legislatures adjourned, suspended or postponed their 2020 legislative sessions and turned their focus to COVID-19
relief," she says. "In particular, we ran out of time to advance legislation in Connecticut and Georgia. Additionally, interim sessions in Tennessee and Utah may not address the respective surgical smoke bills until later this year."
— Joe Paone
Oregon
An effort to reintroduce a 2019 bill this year as HB 4064 was unable to get a committee hearing. Oregon's 2020 legislative session was a very short 45 days with quick turnaround and tight timelines
for all legislative priorities. The legislature directed stakeholders to work on education and awareness of the hazards of surgical smoke in 2020.
California
Cal/OSHA is accepting comments on proposed regulations.
Utah
AORN and local nurse advocates testified in support of SB 105 in February, but the committee did not take a vote. The legislation has moved to the upcoming interim session in the fall for further
study.
Colorado
A bill was signed into law in March 2019. It goes into effect in May 2021.
Iowa
HSB 510 was introduced in the State Government Committee, but the legislation did not move out of committee during the 2020 session. AORN and stakeholders agreed to meet this summer to discuss a bill
for 2021.
Illinois
SB 3753 was introduced in February, but the bill didn't make it out of committee before the deadline. The legislative session was also interrupted by the pandemic.
Tennessee
A bill was forwarded for further study to the interim summer session, scheduled to convene June 1. That session is expected to focus on COVID-19 before taking up other interim legislation this
fall.
Kentucky
The Senate passed SB 91 unanimously in February. It was sent to the Kentucky House Health and Family Services Committee, but not brought up for a hearing. before the legislature adjourned.
Georgia
SB 347 was introduced and heard in the Georgia Senate Health and Human Services Committee in March. AORN worked with the Georgia Nurses Association to support grassroots efforts to advance the
legislation. The bill did not get moved to a summer study session before the legislature suspended its session in response to the pandemic.
New Jersey
AB 3982 was ready to be introduced when the General Assembly temporarily suspended its 2020 session due to COVID-19. Now reconvened, the bill has been introduced. However, COVID-19 relief and
the state budget have put it on the back burner.
Connecticut
HB 5421 was introduced by the Public Health Committee in March. Scheduled and then re-scheduled for a hearing, it didn't advance because the General Assembly suspended its session shortly after
due to COVID-19.
Rhode Island
Law went into effect January 2019.
.svg?sfvrsn=be606e78_3)

.svg?sfvrsn=56b2f850_5)