In the midst of the coronavirus pandemic, members of your surgical team must wear the right level of PPE to protect themselves from exposure to COVID-19. Too little protection, and they'll be unnecessarily exposed to the coronavirus. Too much, and they'll burn through precious PPE supplies in no time.
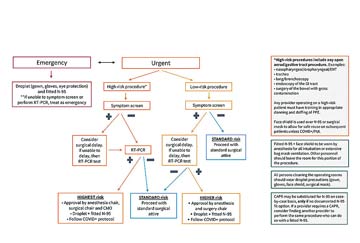
Joseph D. Forrester, MD, MSc, a clinical instructor of surgery at Stanford (Calif.) Health Care, created an easy-to-use algorithm designed to right-size the level of PPE staff wear based on the urgency of the procedure, the risk of the patient having COVID-19 and the likelihood of the patient transmitting the virus to a member of your team.
The algorithm was developed by an interdisciplinary team of stakeholders who prioritized safe patient care, protecting surgical professionals and rationing the use of PPE. Dr. Forrester relied on his experience as an epidemic intelligence officer for the CDC to help guide the algorithm's development. For practical reasons, it's easy to apply; the team's goal was to have the guidelines created by the PPE taskforce, ratified by hospital leadership and implemented within 72 hours. He says leadership from all service lines must be involved in implementing the algorithm's steps.
To determine the level of PPE needed for a particular case, refer to the flow chart (opposite page). The first step is to decide the surgery's level of risk, which depends on the anticipated viral burden at the surgical site and the likelihood that a procedure would aerosolize the virus. High-risk cases include any involving the open aerodigestive tract such as nasopharyngeal and oropharyngeal procedures; bronchoscopy; endoscopy of the GI tract; and surgery of the bowel with gross contamination.
Next, consider the results of the patient's screening for symptoms of COVID-19 (fever, cough, sore throat). Surgical teams can wear standard surgical attire during surgery performed on patients who do not present for surgery with symptoms, according to the algorithm. If the patient does screen positive for symptoms, consider delaying the case or proceeding with staff wearing the highest level of barrier protection.
Patients who screen positive for symptoms at Stanford Health are subjected to in-house reverse transcription polymerase chain reaction (RT-PCR) testing, which detects presence of the coronavirus. Dr. Forrester concedes many facilities don't have immediate access to such resources. "Much of the PPE triage is based on COVID-19 testing," says Dr. Forrester. "Facilities that don't have access to effective testing must operate with more stringent PPE protocols in place."
PPE availability, anticipated burn rates and supply chain disruptions may require modification of the algorithm, according to Dr. Forrester. For example, there was a nationwide critical shortage of N95 masks when he was creating the algorithm. Dr. Forrester's team mandated that staff wear face shields over the masks to protect the masks from excessive soiling and conserve supplies. At the completion of the case, the face shields could be disinfected and the N95 masks reused.
.svg?sfvrsn=be606e78_3)
.svg?sfvrsn=56b2f850_5)