The best-laid patient positioning plans often go awry as soon as surgeons walk into the OR. "It's often done according to their preferences, which is a problem," says Lisa Bachetti, BSN, RN, CNOR, CNIV, staff nurse at Penn Medicine at University City Ambulatory Surgery Center in Philadelphia, Pa. "We have four surgeons who want patients positioning differently for shoulder arthroscopies. Three want patients in the lateral position, but each has slightly different variances on how they want it done. The other surgeon prefers to operate on patients in the beach chair."
The issue at Ms. Bachetti's facility was a lack of detailed positioning information for OR staff to reference. "A surgeon's preference card would note "?beach chair position,'" she explains. "But that's all it would say. As a nurse, I'd position patients how I'd want it done, but that wouldn't be how the surgeon liked it. There were so many small differences we had to manage."
Ms. Bachetti set out to develop surgeon- and procedure-specific educational tools that could be accessed easily in the OR. She gathered all the surgical nurses and asked them which types of cases had the most frequent positioning variations from surgeon to surgeon. Turns out, it was shoulder and knee procedures.
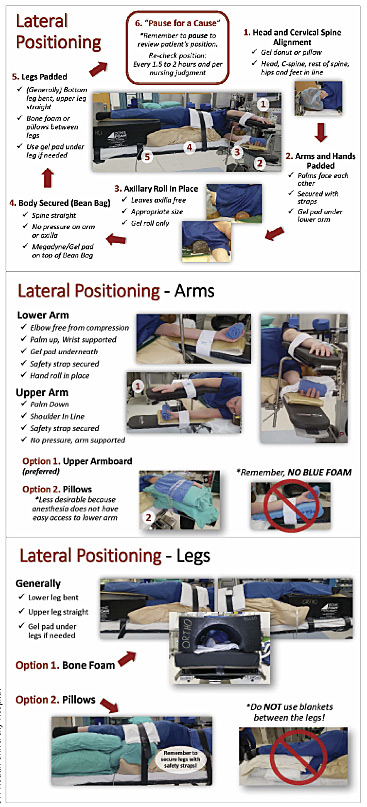
Ms. Bachetti then approached the facility's orthopedic surgeons to tell them about her project, and asked them about their specific positioning preferences, and their rationales for them. Once she collected that information, she created PowerPoint slides for each surgeon and the procedures they performed. But the idea wasn't to put them in a binder; she wanted the information easily accessible to the surgical staff.
She met with the hospital's IT department to develop a sharable file on a web-based collaborative platform. Now OR staff members can easily obtain positioning information through computers in the OR. "Staff access a list of our orthopedic surgeons," says Ms. Bachetti. "They click on a surgeon's name, and in his file are the procedures he frequently performs — ACL, rotator cuff, shoulder arthroscopy. Clicking on a procedure type displays the surgeon's digital preference card, which includes pictures of how they want patients positioned for the procedure."
.svg?sfvrsn=be606e78_3)



.svg?sfvrsn=56b2f850_5)