Active patient warming prevents hypothermia and many related complications such as cardiac trouble, impaired immune function, increased risk of infection and lengthier post-op stays. But you have to worry about an entirely new set of safety issues when staff don't follow proper warming protocols. Unfortunately, that occurs far more often than it should.
"Warming devices aren't benign pieces of equipment designed solely for patient comfort," says Michelle Feil, MSN, RN, CPPS, WCC, clinical practice leader at Penn Medicine in Philadelphia, Pa. "These are therapeutic medical devices that carry a real risk for patient harm."
Ms. Feil would know. She authored a Pennsylvania Patient Safety Authority report that analyzed 278 harmful or potentially harmful events associated with patient warming devices (osmag.net/7yCKNk). Here are a few of the real-world warming mishaps she discovered.
- Thermal injuries. The most frequently reported type of patient harm in Ms. Feil's report come in a variety of forms, but they nearly all stem from the same root cause: Using warming devices in a manner that's not consistent with the manufacturers' Instructions for Use (IFU). For example, the report cited an example of a patient who'd been lying directly on top of a warming blanket during an appendectomy, which resulted in reddening of his skin and a small, reddened area on the right buttock. That usage went against the blanket's IFU, which specifically stated patients should never be positioned on top of the blanket, that they should only be covered by it.
Then there's the extremely dangerous practice of "free hosing," where the hose of a forced-air warming device is placed underneath surgical drapes or the blanket of a patient's bed or stretcher. This off-label use has resulted in a number of cases of serious patient burns because of the change in the distribution of the heat.
"If you place a hose underneath the drapes, you're focusing a very concentrated amount of heat in one area," says Victoria M. Steelman, PhD, RN, CNOR, FAAN, a patient safety expert and an associate professor at the University of Iowa College of Nursing in Iowa City. "And patients generally can't tell you if they're being burned."
Another seemingly harmless free-hosing practice that is anything but: Putting the hose under a blanket to warm the bed when the patient isn't on it yet. "That's not filtered air," says Dr. Steelman. "The practice creates aerosolized fibers from the blanket, and that's not a prudent thing to do."
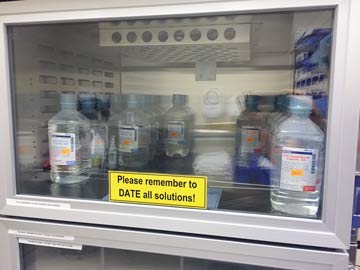
It's not just the warming devices and blankets that are being used incorrectly and opening up patients to safety risks. Warming IV or irrigation fluid is a useful adjunct to patient warming that has shown to be effective in preventing hypothermia when combined with other warming methods. But facilities sometimes warm IV fluids in warming cabinets designed specifically for cotton blankets, a big no-no as the high temperatures have led to patients being burned.
.svg?sfvrsn=be606e78_3)

.svg?sfvrsn=56b2f850_5)