Cataract surgeons who claim they're not worried about piercing the posterior capsule with a sharp instrument or oscillating phaco tip? "They're either lying or retired," says Uday Devgan, MD, a cataract surgeon in Los Angeles, Calif.
While posterior capsular ruptures are rare — it's estimated they occur in 6% of novice surgeons' cases and in less than 1% of experienced physicians' procedures — they increase the risks of endophthalmitis and cystoid macular edema, adverse events that adversely affect patients' post-op vision. But a rupture impacts more than quality outcomes. Your case costs and profit margins suffer collateral damage. Consider:
- Surgeons must open 2 or 3 more tubes of viscoelastic to keep the tear from expanding, and prevent or limit vitreous loss.
- They must use intracameral preservative-free triamcinolone during clean-up of the tear to increase visualization of the vitreous that prolapses into the anterior chamber.
- They must open an anterior vitrectomy pack, use acetylcholine chloride intraocular solution to constrict the pupil, and administer additional steroids or antibiotics.
- And your surgeons might have to insert a three-piece IOL, which is less likely to expand the tear, instead of a two-piece IOL.
All of those steps and additional supplies more than double the duration of surgery and inflate your case costs, says Dr. Devgan, stressing that you can't afford to waste minutes and dollars in a volume-driven specialty with razor-thin profit margins.
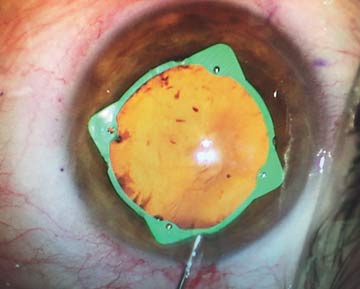
Fortunately, advanced phaco fluidics, femtosecond-lasers and mydriasis-maintaining drugs can help prevent tears from occurring.
.svg?sfvrsn=be606e78_3)
.svg?sfvrsn=56b2f850_5)