We've always known about the hidden bacterial threat in your OR's anesthesia work area, the microbes lingering on the anesthesia machine and the pathogens on the laryngoscope handle that didn't get a full cleaning between cases. Then there's the anesthesia provider's hands — be they bare or overdue for a fresh pair of gloves — as they intubate the patient, and prepare and deliver IV medications. And yet we're still struggling to prevent the infections that originate from that challenging environment. Here are 3 takeaways from The Society for Healthcare Epidemiology of America's (SHEA) new guidance (osmag.net/yGWfT5) on infection prevention in the anesthesia work area.
- Home
- Article
Anesthesia Alert: Anesthesia's Infection Control Challenges
By: L. Munoz-Price, T. Andrew Bowdle
Published: 3/14/2019
It's time for your providers to clean up their acts - and their workstations.
Hand hygiene
We recommend anesthesia providers follow the World Health Organization's (WHO) My 5 Moments for Hand Hygiene (osmag.net/7PBqyD): cleaning their hands before touching a patient, before clean/aseptic procedures, after body fluid exposure/risk, after touching a patient and after touching patient surroundings. Following the WHO protocols to the full extent may be difficult — or maybe even impossible — but we want providers to wash their hands more often.
One simple switch can help: Add a hand gel dispenser to the anesthesia work area. A surprising number of anesthesia providers don't have access to hand sanitizer in their immediate workspace. Fire codes come up from time to time as an excuse, but you can adhere to fire codes and still have a dispenser in the anesthesia work area.
We also recommend providers double-glove during airway management and discard the outer gloves immediately after airway manipulation. As soon as possible, they should remove their inner gloves and wash their hands.
Turnover rush
OR managers want to shorten turnover times, but there's no fast way to clean the anesthesia workspace. The anesthesia cart is its own beast. You set yourself up for problems if you're going into the cart's drawers with dirty hands or you're not giving the instruments the full disinfection they need. The computer keyboard, the monitor and mouse, the reusable patient-monitoring equipment and blood pressure cuffs are just a few potential hosts for microorganisms.
Look at your laryngoscopes. Are you giving the scopes the necessary high-level disinfection? It's easier to clean the blades, but the handles can be time-consuming. Single-use laryngoscopes have improved over time and may be worth considering. The single-use scopes don't pose the same concern when it comes to battery life and wear and tear. Evaluate the time you're taking to clean reusable laryngoscopes and the waste that comes from single-use options.
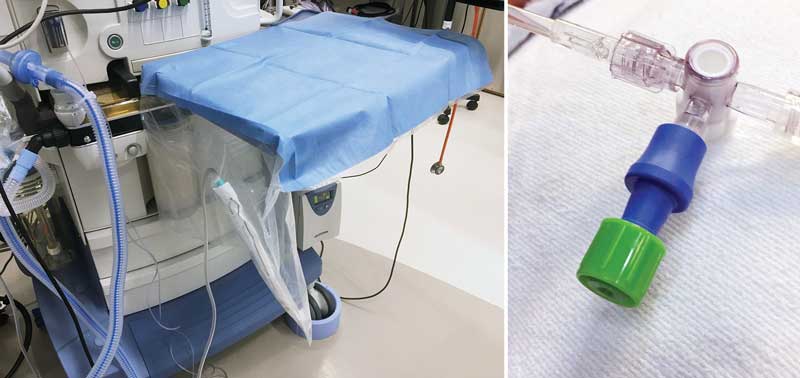
The anesthesia machine poses another turnover challenge, with its knobs, handles and overall bulk. Plastic anesthesia machine covers could help guard against cross-contamination, but we need more research showing they work.
Ports and stopcocks
Any time you inject IV drugs, you should think about the potential for contamination. Ports and stopcocks are 2 common culprits for potentially pathogenic bacteria. As a rule, anesthesia providers should only use disinfected ports for IV access. You can disinfect ports with a sterile, alcohol-based wipe before each use, but we recommend using isopropyl alcohol-containing caps. This option makes ports available whenever you need them. It's simpler and safer. Stopcocks should have closed injection ports installed to convert them into "closed ports," as well. Cap your stopcocks with an isopropyl alcohol cover and you're good to go.
A clear threat
We can do better when it comes to hand hygiene, cleaning between cases, and capping ports and stopcocks, but we need to be thinking bigger. How can we redesign the anesthesia machine so it's easier to clean? What research questions do we need to ask about the threat of infection? We want to design improvements that make the OR safer. It's a big task, and one that can get overlooked in the daily grind of patient care. We need more research looking at the possible contamination of anesthesia equipment (and providers) and its impact on clinical outcomes.
So why don't we know more? For one thing, we don't have the urgency. When a patient acquires MRSA, it's hard to pinpoint when the infection happened. It could have occurred anywhere in a 30-person chain of interactions during an outpatient surgery stay. It could stem from a single instrument in the anesthesia drawer or a provider who didn't wash his hands frequently enough. The delay between exposure and infection makes it harder to hold ourselves accountable, but we should still try. If we could only see the bacterial threats living in our ORs, we'd all be rushing to get started. OSM

Here are 5 examples of when anesthesia providers should perform hand hygiene.
- 1. Before aseptic tasks, such as inserting central venous catheters, inserting arterial catheters, drawing meds and spiking IV bags.
- 2. After removing gloves.
- 3. When hands are soiled or contaminated.
- 4. Before touching the contents of the anesthesia cart.
- 5. When entering and exiting the OR (even after removing gloves).
.svg?sfvrsn=be606e78_3)
.svg?sfvrsn=56b2f850_5)