In our busy hospital, patients start their surgical journey in pre-op bays, where nurses place IVs, check vital signs and perform clinical assessments. Patients are then moved to a surgical holding area adjacent to the ORs until it's time for surgery. Previously, we wrapped patients in warmed cotton blankets in the pre-op area and only began active warming measures in the holding area.
The decision to initiate active warming in pre-op and continue applying the methods straight through to PACU actually began as a lean strategy aimed at reducing the significant laundry expense our hospital incurred from washing cotton patient gowns and the countless cotton blankets we used to warm patients throughout their stay. (Quick tip: If you're unaware of the number of blankets your staff goes through to keep patients warm and comfortable, hang a dated spreadsheet next to your blanket warming cabinet and ask staff to make a tick mark every time they grab a blanket. The number of blankets they use might be eye-opening.)
We replaced cotton gowns and blankets with disposable forced-air warming gowns, which patients slip on in pre-op and wear straight through to discharge. That option works best for us, but there are several effective active warming methods from which to choose, including forced-air warming coverlets, conductive blankets and mattresses placed over and under patients, reflective thermal blankets that trap the patient's own body heat and warm circulating water mattresses.
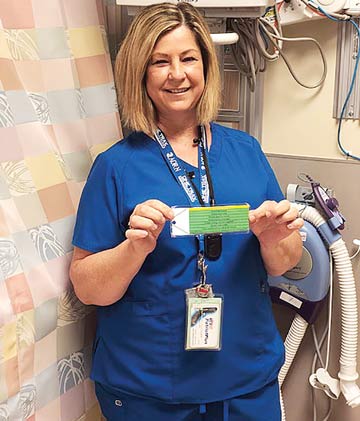
Smaller warming units are mounted on walls next to patient beds in the pre-op and holding areas. These smaller units deliver enough heated air to pre-warm patients, who can adjust the air flow to their comfort, and keep floors clear of tripping hazards in the busy, high-traffic areas.
We note the many clinical benefits of maintaining normothermia on laminated scripts that are attached to each wall-mounted unit (see "Post This Patient Warming Cheat Sheet"). The scripts ensure every staff member who comes in contact with patients, even those who don't regularly care for them in pre- and post-op areas, understand the clinical importance of patient warming and maintaining normothermia. That's where the script comes in handy. Any provider, no matter how well-versed they are with our patient warming protocols can refer to the script when interacting with patients.
.svg?sfvrsn=be606e78_3)



.svg?sfvrsn=56b2f850_5)