The annual American Society of Anesthesiologists (ASA) Anesthesiology conference is the world's largest anesthesia meeting. On a clinical level, I'm here to see the latest products and technology. This is also my chance to chat for a bit with peers I see once a year. It's very flattering that hundreds of my colleagues took the time to listen to my "wisdom and experience" during my refresher course. For me, this conference reaffirms that I'm learning from my peers and sharing my expertise with them.
As anesthesiologists, the 2 biggest things we do are airways — and everything else. With any new device here, I want to see how it would be different from what I already have. Is it an improvement? Is it smaller, faster, cheaper, more efficient? Is the rate of complications lower? I also come here to learn about the latest developments in the drugs we use — old drugs being reintroduced, new drugs just hitting the scene, new indications for existing drugs. Here are some of the more interesting and relevant products I saw roaming the exhibit hall at ASA 2019. OSM
Merck & Co.
Bridion
merckconnect.com
Each single-use vial of Bridion (sugammadex) for reversing neuromuscular blockade contains a concentration of 100 mg/mL of sugammadex. Dosing is based on actual body weight and depth of block — 2 mg/kg for a moderate block and 4 mg/kg for a deep block. Vials include a peel-off label that you can apply to the syringe. Routine co-administration of an anticholinergic agent is not required, says the company. Bridion is contraindicated in patients with known hypersensitivity to sugammadex or any of its components.

IntelliGuard
IntelliGuard Anesthesia
ig.solutions
Manually keeping track of my drug supplies in the OR, or even using a bar-coded system, can be time-consuming and lead to inaccurate inventories and breaks in the chain of custody, which are key issues when handling controlled substances. So-called “smart medication management carts” like this present a better — if more costly — way to manage medications by automating the process end-to-end and keeping track of medication supplies centrally. This cart combines hardware, software and analytics powered by Radio Frequency Identification (RFID) technology to manage drug inventory more proactively. To prevent theft and abuse, 2-factor identification is required to unlock the drawers, and the clinician name, credentials, date and time are recorded digitally. You can manually enter case information or integrate an EMR to select from a pre-populated list. After you remove the drug and close the drawer, the drawer’s contents are scanned and the medications you removed are associated with the case and provider. Your pharmacy, if you have one, is plugged into the system, knows exactly what you have on hand, and can replenish your supplies before you’re caught empty-handed. This can really simplify things for both clinicians and administrators, and provide more accurate documentation, but be advised, these machines are expensive — I didn’t get a price from this vendor, but they usually cost in the tens of thousands of dollars.
Medtronic
McGrath MAC Video Laryngoscope
medtronic.com
For me, this product's value is all about “line of sight.” The screen is right on the handle, so I’m never looking away to the side. That makes it much easier to insert the laryngoscope on the first attempt, especially in situations where the patient has a difficult airway. The company promises better glottic visualization than traditional Macintosh laryngoscopy, reduced intubation times, greater ease of use and higher intubation success rates compared with other video laryngoscopes.

Masimo
Radius PPG
masimo.com
This wireless and wearable pulse oximetry sensor solution for patient monitoring removes the need for a cabled connection to a monitor. Patients can thus move freely and comfortably throughout your facility or their home while still being continuously monitored, and they don’t need to physically disconnect and reconnect to the system. Radius PPG (short for photoplethysmography) is comprised of a battery-powered single-patient-use adjustable wrist-strap sensor (which can be of various types and is attached with adhesive tape), a reusable Bluetooth-enabled chip that stores patient data and a wireless receiver with monitor. The sensor’s integrated battery lasts about 4 days and stores up to 4 days of patient data. When a patient leaves your facility, you really don’t want to totally disconnect from them — but we’d also like them to recover at home to cut costs. With this system, you could monitor them at home with real-time data, and using that information, you can positively impact their behavior. Let’s say the patient is falling asleep and her oxygen is decreasing. I could be alerted to this information remotely and get somebody to the house to check on her. Maybe they need a breathing treatment, or need to skip their pain medication.
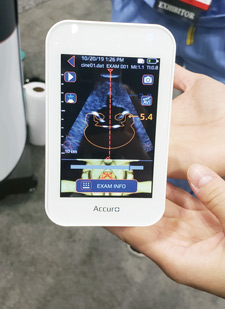
Mindray North America
TE7 Ultrasound System Crystal Series
mindraynorthamerica.com
To look closely at the heart without opening the chest, we’ve traditionally used transesophageal echocardiography, which requires placing a probe down the patient’s esophagus. This product is transthoracic, so it’s non-invasive. You can use ultrasound to see really good images without sticking a probe down somebody’s throat, which creates potential complications. If I can see from the outside what I could only see from the inside before, it really helps, and these images are impressive. This technology automatically detects needle angle and improves visibility on both linear and convex transducers during interventional procedures. You also have navigation technology to visualize the needle’s tip and trajectory. All in all, it’s safer and it appears effective.

Through The Cords
Total Control Introducer
ttcmed.com
For anesthesiologists, a recurrent problem — and a great source of stress — is managing difficult airways, especially in high-BMI patients and those with sleep apnea. It’s the balancing act of anesthesia. Patients can die if you’re unable to ventilate them. Sometimes in these urgent situations, anesthesiologists panic and get fixated on intubation. My recommendation in these situations is not to immediately intubate, but to take a step back, bag mask ventilate and buy time. Our most important skill is ventilation, not intubation; I keep drilling this into anybody who will listen. To me, the most common preventable cause of aspiration is premature attempts at laryngoscopy.
Sometimes, though, intubation is the only option. This product offers an intriguing approach to addressing difficult airways and first-pass failure in emergency intubations by turning your video laryngoscope into a difficult airway management system. The Total Control Introducer has a flexible shaft, a tip that articulates both up and down, and a color-coded depth control system, as well as a removable pistol-grip handle that lets you place the tube over the introducer once in place in the trachea, removing the need to preload the tube on the device. The idea is to give the anesthesiologist precise introducer tip control at the level of the vocal cords. The vendor positions it as a rescue tool that’s easy to reach for when needed, and a disposable alternative to more expensive reusable fiberoptic bronchoscopes.
.svg?sfvrsn=be606e78_3)












.svg?sfvrsn=56b2f850_5)