Lessons Learned From a Renowned Team Physician
As a well-known team physician for not one but two professional Chicago franchises — the Bulls and the White Sox — Adam Yanke, MD, PhD, sees his fair share of non-athlete...
This website uses cookies. to enhance your browsing experience, serve personalized ads or content, and analyze our traffic. By clicking “Accept & Close”, you consent to our use of cookies. Read our Privacy Policy to learn more.
By: Jared Bilski
Published: 12/19/2019
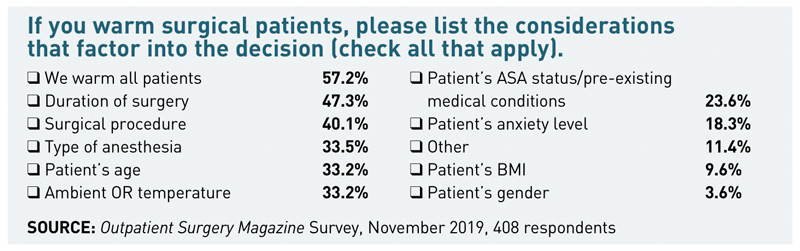
It should come as no surprise that most outpatient facilities warm their surgical patients. After all, there's an ever-growing mountain of evidence that says warming prevents hypothermia as well as many related complications like cardiac trouble, impaired immune function, increased risk of infection and lengthier stays in recovery. Plus, it's a proven patient-satisfier. What may surprise you, however, is how, when and why your peers warm patients. These are the details we aimed to uncover with our survey of more than 400 facility leaders.
One of the most notable survey findings: 63.2% of facilities said they "always" warm surgical patients. That's a sizable jump from the 52.7% of facilities that reported "always" warming patients back in 2013, the last time we surveyed readers on this topic. Overall, however, the percentage of readers that warm patients at least "occasionally" has remained largely unchanged, 90.1% in 2019 and 90.2% in 2013.
Just 2.3% of readers said they "never" warm patients, and the bulk of these respondents came from facilities that were only doing extremely short procedures like cataracts.
In terms of when they warm patients, 68.8% of respondents warm patients pre-operatively (a big jump from the 33.2% who responded this way in 2013); 89.3% warm intraoperatively; and 72.1% warm patients post-operatively. For the facilities that practice prewarming, 50.6% do it for 30 minutes or longer, while around one-third (34.6%) of facilities prewarm patients for less than 30 minutes. For some, prewarming isn't based on a standardized time frame like 30 minutes or less, but on a number of factors such as patient choice, or anesthesia and procedure type.
For example, DeShawn Bhooshan, RN, HCRM, CNOR, the clinical nurse manager at USF Health Endoscopy and Surgical Center in Tampa, Fla., says that in pre-op all patients "get a warm blanket upon arrival and if it's a general anesthetic case or a case other than eyes, they get a full-body forced-air blanket."

Our survey found that readers predominantly use 2 methods to warm patients: a forced-air warming system (Bair Hugger) or a cotton blanket pre-warmed with a blanket warmer, cited by 83.2% and 81.4% of respondents, respectively. Among the other warming methods: 6.61% use a spinal underbody blanket (or thermal mattress or bed pad on which the patient lies), 3% use some type of radiant warming device and 1.5% use a conductive polymer fabric that warms the patient from above and below simultaneously. Another 6.3% cited "other" and listed a variety of warming methods including warm compresses, hot packs and a Mylar blanket.
Nearly two-thirds (63.9%) of respondents warm fluids. By far, the top fluid-warming method cited was a warming cabinet (84.8%). Nearly one-third (32.7%) use "a warming device as the fluid is administered intravenously."
At the heart of this survey is a simple question: Why do you warm patients? The top reasons readers gave for warming patients were to "make patients comfortable/prevent shivering" (92.4%) and to "prevent hypothermia and its clinical complications" (79.9%). In addition, 52.7% warm patients to prevent surgical site infections and 51.2% do it to reduce recovery/PACU times. Of course, safety is always paramount for facilities, so it's no surprise many readers cited preventing surgical site infections and hypothermia as primary reasons for their warming protocols. But the patient satisfaction impact simply can't be overstated, so it's very telling that the top reason readers gave for warming patients was to make them comfortable and prevent shivering. After all, comfort is a key patient-satisfaction metric.
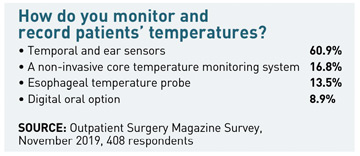
"I've always felt that when patients are warm, they're happier and feel better taken care of," says Pamela Borello, BS, RN, CNOR, CSSM, a nurse at Michigan Cosmetic Surgery Center in West Bloomfield. And when patients feel better, they're more likely to give your facility a better overall review, adds Ms. Borello. At Michigan Cosmetic Surgery Center, patients are warmed at every phase of the surgical journey — pre-operatively (with cotton blankets warmed with a blanket warmer "at the highest temperature setting for blanket warmers"), intraoperatively and post-operatively — and their temperatures are monitored via temporal and ear sensors.
While Ms. Borello says patient safety is her facility's top priority, she also understands that patients have different concerns when they're coming out of anesthesia. "When patients wake up, they're not worried about SSIs," says Ms. Borello. And though you may not find clear evidence directly linking warmer, more comfortable patients and reduced pain, Ms. Borello has seen this connection firsthand. Patients' pain just seems less when they're warm. They're not shivering, they're not stiff. You just can't relax when you're in the PACU shivering, Ms. Borello says.

It's impossible to talk about patient warming without at least addressing the state of the 3M lawsuits and their effect on outpatient facilities. As Outpatient Surgery reported in August (osmag.net/YNnu4Q), a federal court dismissed more than 5,000 lawsuits against 3M that claimed its Bair Hugger device was responsible for infections suffered by patients during surgery. The dismissal is the latest in a 6-year legal battle between plaintiffs and 3M, and comes on the heels of the Minnesota Court of Appeals upholding a state court order that dismissed 61 similar lawsuits against the company's patient warming system. The judge's memorandum does not impact 2 similar state court cases against 3M's Bair Hugger (one in Missouri and one in Texas), which are ongoing.
We asked readers whether the lawsuits against the Bair Hugger system impacted their attitudes toward and/or their use of forced-air warming systems. While most readers (93.3%) said the lawsuits did not have an impact, 6.7% said the legal action against the most popular patient warming system on the market did affect their attitudes, policies or both. And that small percentage had some interesting things to say about the latest chapter in the forced-air warming controversy. A source from a facility in Nebraska who asked to remain anonymous said, "the lawsuits definitely made our surgeons a bit hedgy. There had been concerns about infections for years, and we made a safety decision not to go with the Bair Hugger long before the legal action began. But for us, the lawsuits showed our concerns were justified and that we made the right decision."
At this point, the question shouldn't be Why should you warm patients? Rather, the question should be Why wouldn't you? Perhaps, Sherry Goldstein, RN, MA, BSN, director of nursing and perioperative services for Loyola-Gottlieb Memorial Hospital in Melrose Park, Ill., put it best when she said, "If you read and understand the literature and guidelines on patient warming, how can you say I don't want this for my patients? How can you deny them the best and safest care?" OSM
As a well-known team physician for not one but two professional Chicago franchises — the Bulls and the White Sox — Adam Yanke, MD, PhD, sees his fair share of non-athlete...
George Dugan, CRNA, RN, an anesthesia provider for Temple University Health System in Philadelphia, is no stranger to pain. His patients frequently suffer for months...
In the world of hand and wrist surgery, the Wide-Awake Local Anesthesia No Tourniquet (WALANT) technique has revolutionized both pain management and the patient...