Renowned neurosurgeon John Boockvar, MD, strides into an operating room at Lenox Hill Hospital and greets members of his surgical team as they gather in a loose circle. "Let's take a moment to be mindful," says Dr. Boockvar, one of the stars of the Netflix docuseries Lenox Hill, a compelling look at the everyday lives of four physicians who work at the storied hospital on Manhattan's Upper East Side.
"Everyone relax and close your eyes," instructs Dr. Boockvar, who radiates a sense of calm. "Wiggle your toes and roll your shoulders back. Be here in the present. Take a deep breath in, hold it at the top, exhale."
Dr. Boockvar pauses in the middle of the now silent room. He's entered flow state, the heightened awareness needed to perform difficult tasks effortlessly and with complete focus. It's time to remove a worrisome growth from the patient's right frontal lobe and Dr. Boockvar is emotionally, physically and mentally present. He's ready to cut. "OK, let's roll."
Flow state is the culmination of grit and mindfulness — the three principles of "gritflowness," a term Dr. Boockvar coined to describe the techniques he uses to remain focused and calm when faced with the unimaginable stress of performing complex brain and spine procedures where the line between success and failure is measured in microns.
"It takes grit and mindfulness to develop the muscle memory needed to reach flow state," says Dr. Boockvar. "You need to commit to making mindfulness a part of your life, and dedicate the time and effort to accomplish it."
Grit involves deliberate practice and single-minded commitment to master a skill. Michael Jordan shot thousands of jumpers so he could drop 55 points on the Knicks in Madison Square Garden. Tiger Woods wore out practice ranges on his way to winning his first U.S. Open at Pebble Beach by 15 strokes. ?Dr. Boockvar spent endless hours in cadaver labs during medical school performing new surgical techniques under a mentor's watchful eye before eventually becoming one of the best neurosurgeons in the world.
"In order to reach peak performance, you have to practice a skill until it essentially becomes unenjoyable," says Dr. Boockvar. "Over time, you develop a high enough skill set to meet any challenges that come your way."
Mindfulness is being fully present in the moment, without worry of past events or future possibilities. It's an essential skill for managing the inevitable stress of everyday life inside and outside of the OR.
"Dwelling on past failures, or thinking about all the responsibility we're given and feeling like we have little control over situations are the daily challenges to mindfulness," says Dr. Boockvar.
He refers to three universal possessions when describing how to become fully aware. "My phone is a problem and my wallet can cause stress, but my breath can help me," says Dr. Boockvar. "Focused breathing is a tool that's always available."
Practicing mindfulness, even for a few minutes each day, is scientifically proven to prevent burnout caused by the cumulative effect of chronic stress. The amygdala, the brain's center for emotional behavior, is "hot" when you're anxious or depressed and "cold" when you're calm and relaxed. "Mindfulness and meditation are proven ways to cool down the amygdala," says Dr. Boockvar.
The 4-7-8 breath — inhaling through the nose for four seconds, holding it in for seven seconds and exhaling slowly through the mouth for eight seconds — is the ideal initial step on the path to mindfulness. "If you do it for two minutes a day, you're well on your way," says Dr. Boockvar.
He came up with gritflowness about five years ago as a way to remind himself of the grit and mindfulness needed to enter flow state as a husband, father and surgeon. His interest in the philosophy's core concepts began much earlier when he developed a fundamental knowledge of neuropsychopharmacology and a passion for cognitive neuroscience as an undergrad at the University of Pennsylvania in the early 1990s. But it wasn't until fate handed him a copy of "Full Catastrophe Living," the bible of mindfulness teaching, that he fully embraced mindfulness — long before the concept became a boardroom buzzword and social media hashtag.
Dr. Boockvar has added mindful moments to surgical time outs to build team unity and create a sense of group calm. He asks his colleagues to focus on their breathing for 10 or 15 seconds before procedures begin. "We check the patient and confirm the details of the operation, but we also need to check in on the well-being of the staff," he says. "It introduces the concept of mindfulness to members of the team, and hopefully inspires them to begin training, even for just a few minutes a day."
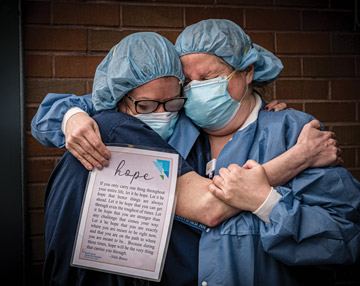
Being centered and fully present in the moment have never been so important. Dr. Boockvar points to the 60% burnout rate among surgical professionals and says the COVID-19 pandemic has only increased the professional and personal stress they face on a daily basis. "We come to work with human emotions, and we all need a little help," says Dr. Boockvar. "It's important to acknowledge stress and understand there are simple ways to manage it. When you integrate the three concepts of gritflowness, you end up in the perfect state of mind." OSM
.svg?sfvrsn=be606e78_3)


.svg?sfvrsn=56b2f850_5)