No matter how hard one tries, the skin simply cannot be made sterile. It can, however, be made surgically clean. Optimizing the skin’s cleanliness prior to surgery is the target that every provider should focus upon. To achieve a consistent perioperative antisepsis process, everything from the products chosen to the application techniques to the training conducted, should be standardized. Otherwise, how can one measure quality from one patient to the next?
- Home
- Article
Simplify the Skin Prepping Process
By: Peter Graves, BSN, RN, CNOR
Published: 5/19/2022
Standardized protocols render incision sites as clean as possible before surgery.
Putting a plan in place
I’m a firm believer in an interdisciplinary team approach to surgical skin antisepsis standardization. Start by gaining consensus from infection prevention, perioperative services, purchasing, surgeons, nurses and anesthesia providers. Then, define exactly what your facility’s process will include. For instance, will part of your process include nasal decolonization or targeted more complex cases (total joints, spine, etc.)? If so, will it be universal decolonization? What about preoperative bathing? Both practices should be outlined in policies for prepping the skin for surgery. At the very least, patients should bathe the night before and morning of surgery using soap or an antiseptic, according to AORN guidelines. The focus of these efforts is to reduce bacteria, soils and oils from the skin.
Hair removal needs to be incorporated into prepping protocols. Make sure it’s emphasized — in policies, training and verbally — that all necessary hair removal must be done outside the OR.
Like all good infection control protocols, regular ongoing assessments are necessary to pinpoint compliance — and variability. Communicate areas of needed improvement with the frontline staff and if there are any issues, correct them immediately. Reinforce performance problems that were identified and conduct training and retraining if necessary. Whenever changes to your protocol are implemented, everyone from brand new employees to veteran staff members must be retrained to guarantee you have a consistent process in place to reduce variability and lower infection rates. Reducing variability allows for better measurement of results and a lower infection rate. For instance, several years ago, I worked with a facility to analyze the cause of infection occurring during C-sections. We assessed all aspects of care, from admission until the time of discharge, and found staff were using an inadequate number of applicators to prep the patient’s abdominal wall prior to surgery. Infection rates dropped when they started applying the recommended volume of the prepping product according to the manufacturer’s instructions for use (IFU). It pays to analyze your process regularly, so you can assess the effectiveness and recalibrate it as needed. Having a standardized process makes it that much easier for you to measure outcomes without variability.
Selecting a skin antiseptic can be challenging when you’re trying to balance evidence-based research, clinical guidelines, cost and staff experience, but these AORN recommendations should factor heavily in the decision:
- Assess the patient for contraindications. Determine if potential allergic reactions or the specific anatomy being prepped precludes the safe use of the agent you intend to apply.
- Use an alcohol-based antiseptic solution unless it’s contraindicated. Alcohol is the best broad-spectrum bactericidal agent we have. When it’s combined with a secondary agent or functional excipient, it provides both immediate and persistent antimicrobial activity.
- Selection of antiseptics should be based on the anatomical location. Bodies have moist, dry and oily areas. Each of those areas have different microbiota naturally found on the skin, and each of those areas may respond differently to the same antiseptic. Therefore, more than one agent might be needed to prep an individual patient.
— Peter Graves, BSN, RN, CNOR
Product selection pearls
Once you’ve decided what the skin prepping protocol will cover, standardization will depend on the product you select (See “3 Keys to Picking the Right Agent”). AORN guidelines recommend “alcohol-based antiseptic unless it is contraindicated.” When you’re prepping the skin, you must understand the skin’s function, the importance of the skin’s natural pH and how it will change when an antiseptic agent is applied. Any agent with alcohol, iodine or chlorhexidine can irritate the skin. But so can your everyday bar of soap.
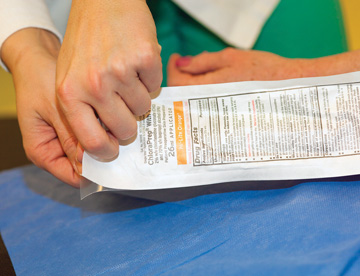
In general, there are two main types of alcohol-based prepping products available on the market. Before being applied, each of these require the skin to be cleaned with preoperative bathing. Some facilities use chlorhexidine gluconate (CHG) wipes in pre-op to further reduce the bacterial count on the skin.
• Alcohol and chlorhexidine gluconate (CHG). This product is applied in a back-and-forth manner for the prescribed time based on the location of the body and the IFU. Its fast-acting broad-spectrum antimicrobial nature provides persistence that’s measured in hours. However, it’s flammable and must be allowed to dry for at least three minutes on hairless skin and up to an hour in hair. Something to keep in mind with all CHG skin antiseptic products: In 2017, the FDA issued a warning letter to healthcare facilities about rare but serious allergic skin reactions.
• Alcohol and iodine povacrylex. This is another fast-acting broad-spectrum antimicrobial agent that provides persistence measured in hours. Again, it’s flammable, so it must be allowed to dry at least three minutes on hairless skin and up to an hour in hair. Some adverse skin reactions have been reported, and the product requires the use of a lotion to remove the film-forming iodine complex from the skin.
It’s worth noting there’s a new alcohol-based broad-spectrum antimicrobial skin antiseptic product slated to hit the market soon: alcohol and functional excipients. Functional excipients are a little different because they focus on the pH of the skin. These functional excipients help maintain the natural pH of the skin, wich inhibits bacterial growth. It is applied to the skin in the same back and forth manner. Since it doesn’t contain chlorhexidine or iodine-based agents, it may be safe for individuals who have a CHG or iodine allergy or intolerance. Like the other two products, the alcohol component means it’s flammable and must be allowed to dry for at least three minutes on hairless skin and up to an hour in hair.
Overall, alcohol-based agents have demonstrated superior efficacy, are easy to apply, have better durability and are more cost-effective when compared to other traditional aqueous-based solutions in various studies. Alcohol is the fastest antiseptic available. It’s a fast-acting agent, while CHG and iodine are considered intermediate-acting agents, meaning it takes a little while for them to render their activity against bacteria and other organisms. In the above products, alcohol kills bacteria (bactericidal) and other organisms on the skin before the secondary agent kicks in. With the prepping agent you select, make sure you can see the tint in the product clearly on all skin tones, as being able to demarcate the skin prep area is important. Once the product is selected, focus on reducing variability in how it’s used and applied to the skin based on the prep manufacturer’s IFU and AORN guidelines.
Skin prepping is a critical infection control practice that needs to be reviewed regularly. How often do you really stop and think about the process when you’re prepping the patient for surgery? It’s easy to go through the steps without focusing on why we’re doing them or whether we’re doing it exactly the same as everyone else. But this is a critical process, and our patients deserve to know we’re doing everything we can to render their skin as surgically clean as possible. OSM
.svg?sfvrsn=be606e78_3)
.svg?sfvrsn=56b2f850_5)